Dr. Abeer Abd ElRhman Elnour Eltilib1
Department of Family Medicine, faculty of Medicine, University of Gezira, Sudan.
E-mail address: Abeert17@yahoo.com
HNSJ, 2023, 4(5); https://doi.org/10.53796/hnsj4527
ORCID: https://orcid.org/0000-0002-7093-2757
Published at 01/05/2023 Accepted at 25/04/2023
Abstract
Quality is the most important issue and the main predictor variable in developing as well as developed countries to achieve the Sustainable Development Goals. Sudan, which is the largest country in Africa, has one of the highest rates of maternal and perinatal mortality, project of safe motherhood in Gezira ,State Sudan lead to reduction of maternal death from 469 per 100,000 live births in 2005 to 139 in 2019, Still in recent years the percentage of maternal death increase so this area need many researches to highlight the problem .: this is a cross sectional study with simple random sampling technique, by got a list of pregnant women attended to the Banat health center per day, assigned each patient a number, wrote each patient number on small piece of paper, ensured good mixing. Then 10 papers were taken. The patients belonging to these numbers were interviewed. This technique was done every working day for two months. Then 400 patients constitute the sample.: regarding age showed that no association between it and service provision[p value 0.992] or Experience of care, satisfaction respectively p vale [ 0.900, 0.618].but there is association between residence and Experience of care. p value[0.050],as same with level of education p value:Still quality of care of pregnant women in Gezira ,State Sudan is suboptimal due to a lot of factors and obstacles as appear in this study lack of investigation ,infrastructure problem clear protocols and guidelines ,educational level, residence.
Key Words: ANC, Pregant Woman, Health Center, Gezira, Sudan
Antenatal care can be broadly defined as encompassing pregnancy-related services provided between conception and the onset of labor with the aim of improving the pregnancy outcome and the heath of the mother or child and providing women and their families/partners with appropriate information and advice for a healthy pregnancy, childbirth, and postnatal recovery. Many maternal and prenatal deaths occur in women with low utilization of antenatal care (ANC) yet the utilization itself is affected by the degree of a client’s satisfaction with that care. Patient satisfaction (PS) is a measure of care quality with the extent to which patients are happy with their health care, both inside and outside of the doctors’ office. The measurement of patients’ satisfaction is a common component of evaluations in quality care. Furthermore, PS gives healthcare providers insight into various aspects of medicine, including the effectiveness of their care and empathy[1]. On the 7th of November 2016, a new set of recommendations had been released as part of the Geneva Declaration of the World Health Organization (WHO). The main aim of the declaration is to attempt the elevation of antenatal care quality, pregnancy process and satisfaction, and the reduction of stillbirth risks along with those of pregnancy complications.
Globally, while 88 per cent of pregnant women access antenatal care with a skilled health personnel at least once, only two in three (66 per cent) receive at least four antenatal care visits. In regions with the highest rates of maternal mortality, such as Western and Central Africa and South Asia, even fewer women received at least four antenatal care visits (53 per cent and 55 per cent, respectively). In viewing these data, it is important to remember that the percentages do not take into consideration the skill level of the healthcare provider or the quality of care, both of which can influence whether such care actually succeeds in bringing about improved maternal and newborn health[2].
Maternal mortality refers to deaths due to complications from pregnancy or childbirth, sub-Saharan Africa and South Asia, account for 86 per cent of maternal deaths worldwide. Sub-Saharan Africans suffer from the highest maternal mortality ratio – 533 maternal deaths per 100,000 live births, or 200,000 maternal deaths a year. This is over two thirds (68 per cent) of all maternal deaths per year worldwide. South Asia follows, with a maternal mortality ratio of 163, or 57,000 maternal deaths a year, accounting for 19 per cent of the global total. Furthermore, regional and global averages tend to mask large disparities both within and between countries [3-4].
There are many socio-economic and cultural factors which act as barriers to the use of antenatal care[5].
Although, it can’t be claimed that antenatal care is the only solution for the high maternal and perinatal death in the developing world, but it can help to reach the Millennium Development Goals for the maternal and child mortality[6].
Sudan, which is the largest country in Africa with 40 million inhabitants, has one of the highest rates of maternal and perinatal mortality[7].
On the other hand there’s there is little published data concerning the use of antenatal care in Sudan[8,9].Although there is project of safe motherhood in Gezira ,State Sudan and lead to reduction of maternal death” The Gezira initiative has led to a remarkable reduction in the maternal mortality ratio (MMR) and in the neonatal mortality ratio (NMR) in Gezira State. The effort has recorded great achievements in Gezira, lowering the MMR from 469 per 100,000 live births in 2005 to 139 in 2019”[10].Still in recent years the percentage of maternal death increase maybe due to drop of all health services in Sudan due to revolutions and a lot of Migration of health providers and so associated factors all this need to be research as to stop Maternal death and increase awareness’ of pregnant with importance of ANC in PHC .
Maternal mortality resulted as a consequence of complications related to pregnancy and birth. Many complications exist before pregnancy and become worsened during pregnancy. About more than 80% of maternal mortalities are due to obstetrics hemorrhaging, infection, hypertension, and unsafe abortion [11].
The high maternal mortality (MMR) rates in some areas consistently reflects the imbalance in health services and the gap between the nations based on the poor and rich divide. More than 90% of the maternal mortalities (MM) take place in low- or middle-income countries, with the majority occurring in the World Health Organization (WHO)-African Region [12].
Quality is the most important issue and the main predictor variable in developing as well as developed countries to achieve the Sustainable Development Goals (SDGs) [13]. But quality is very difficult to define owing to the nature of complex concept and it is very difficult to measure directly [14]. There are many definitions in the literature. Quality is the degree to which services confirm to its intended design (process) [15], the one that provides service at an acceptable cost [16] and the capacity to satisfy the need of the client or patient [17].
In developing countries like Sudan, it is very difficult to make the women satisfied by increasing the number of visits alone [18] as there are limited resources like human power, poor provider training service, poor infrastructure, and administrative weakness at facilities [19]. Still, now Sudan Ministry of Health follows the WHO-recommended FANC visits and the core contents of ANC visits
Materials and Methods
A facility base, cross sectional analytic study, design was used to conduct the study among patients presenting at Baant Health Center in Wad Medani Town, Gezira State, Sudan
between June and September 2022.
A structured data collection tool was developed after carrying out a literature review mainly adapted from the publications.
Since this is a cross sectional study with simple random sampling technique, by got a list of pregnant women attended to the Banat health center per day, assigned each patient a number, wrote each patient number on small piece of paper, ensured good mixing. Then 10 papers were taken. The patients belonging to these numbers were interviewed. This technique was done every working day for two months. Then 400 patients constitute the sample.
CHECK LIST
Item available not available
Facility readiness
- 24hrs availability
- Emergency preparedness
Equipment
- Weighing scale
- Height scale
- Sphygmomanometer
- Stethoscope
- Fetoscope
- Thermometer
- Sterilizer
Medicine
- Tonics (iron ,folic acid) not free
- Calcium tabs
- Anti malaria
- Antibiotics
- Tetanus vaccine
Infrastructure
- Functional ambulance
- Separate room for ANC
- Beds
- Toilet and bathroom facility
- Tape water supply
- Electricity supply
Staff
- General Medical Doctor
- Specialist Medical Doctor
- Heath visitor
- Nurse
- Lab Scientist
- Pharmacist
- Guidelines/Protocols
- Register(separate records for female in reproductive age)
- Health insurance for all female in reproductive age
- Continuous education and training in postnatal care supervision
Number of doctors=2
Doctor Patient Ratio1:15-20
Investigations
Lab facility
- Hemoglobin
- Urine for albumin detection
- Blood grouping
- Ultrasound
- The health center is clean
Results
services provision and Services experience(operational services):
100% (400) of the respondents abdominal examination, fundal level and FHS were provided, 99.2%(397) BP was measured . Regarding check of UG 100% (400) were checked and hemoglobin check in 100%(400 ) of the client, TT was provided in 100%(400),Folic acid was provided to 98.5%(394) of them. About 56.2% (225) were received anti malaria during their pregnancies. In 26%(104) of the respondents U/S for pregnancy was done .
the result showed that the respondents always told about the results of BP,UG , hemoglobin and sometimes about signs of pregnancy and never about the weight and height. About 95.5%(382) of the respondents they can asked any thing they want, 96%(384) treated with respect, 84.2%(337) said that the investigations were available .
demographical characteristics :
Table(1) the distribution of the study participants according to their demographical characteristics (n = 400)
Source: Researcher from Banat health center Wad, Madani ,Gezira -Sudan 2022
Services provision
Table (2) distribution of respondents for Services provision (measurement)(n=400)
| measurement | Yes | No | ||
| N | % | N | % | |
| Height measurement | 15 | 3.7 | 385 | 96.3 |
| Weight measurement | 14 | 3.5 | 386 | 96.5 |
| Blood pressure measurement | 397 | 99.2 | 3 | 0.8 |
| Abdominal examination | 400 | 400 | 0 | 0 |
Source: Researcher from Banat health center Wad, Madani ,Gezira -S
| Measurement | Always | Sometimes | Never | mean | trend | |||
| N | % | N | % | N | % | |||
| Did you tell about the results of abdominal examination | 209 | 54.4 | 132 | 34.4 | 43 | 11.2 | 1.57 | Always |
| Did you tell about the results of weight | 14 | 3.5 | 5 | 1.2 | 381 | 95.3 | 2.91 | Never |
| Did you tell about result of height | 14 | 3.5 | 5 | 1.2 | 381 | 95.3 | 2.91 | Never |
| Did you tell about the result of BP | 231 | 57.8 | 132 | 33 | 37 | 9.2 | 1.52 | Always |
| Did you tell about the result of UG | 204 | 51 | 149 | 37.2 | 47 | 11.7 | 1.61 | Always |
| Did you tell about the result of HB | 308 | 77 | 77 | 19.3 | 15 | 3.7 | 1.27 | Always |
| Did you tell about the signs of pregnancy and childbirth forecast | 96 | 24 | 202 | 50.5 | 102 | 25.5 | 2.02 | Sometimes |
| Did you tell about the mental and physical preparations of pregnancy and childbirth | 90 | 22.5 | 185 | 46.3 | 125 | 31.2 | 2.09 | Sometimes |
| Did you tell about proper nutrition during pregnancy and childbirth | 135 | 33.8 | 179 | 44.7 | 86 | 21.5 | 1.88 | Sometimes |
| Did you tell about the importance of breast feeding and how | 121 | 30.2 | 142 | 35.5 | 137 | 34.3 | 2.04 | Sometimes |
| Realizing importance of ANC | 227 | 56.7 | 159 | 39.8 | 14 | 3.5 | 1.47 | Always |
| Realizing of the importance of taking tonic(folic acid – iron-calcium ) | 315 | 78.8 | 72 | 18 | 13 | 3.2 | 1.25 | Always |
Table (3) distribution of respondents for experience of care(n=400)
Table (4) association between age ,residence and level of education with service provision N
=400
Fig(1) service provision
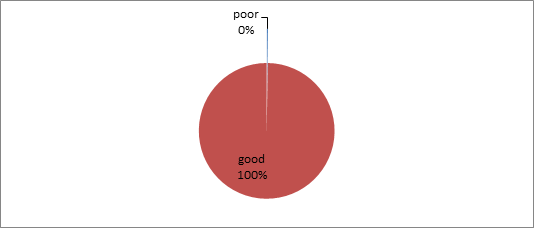
Fig(2) Experience of care
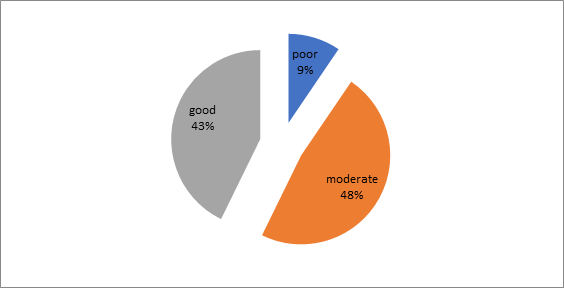
Fig (3) satisfaction
DISCUSSION
This study was done among 400 of women in the reproductive age who visit the HC during June 2022to September 2022,the age group of the study participants from 15 -45 years , majority of them (68.5%)at age group 20-40 years , .This finding is consistent with Study of Maternal health Services in Sudan in 2019 Khartoum[20] .In the study the participants were between the ages of 20 and 42, with a median age of 27years. It seems to be that ANC service seekers are in group of young age mothers.
The findings showed that about 30.8% of the respondent had secondary level of education , while27.8% had level of university , and 4.5% were illiterate .There is strong relationship between educational status of the mother and better access towards ANC , strong relationship between educational status of the mother and experience of care p value was (0.066) . As the findings in study carried out in Pakistan in April 2017 which was found that mother’s education, pointed out that mothers, who had better education, indicate positive inclination to have maternal health care services. [21]
The majority of respondent 55% of them, from the catchment are .There is significant correlation between the resident and services provision ,which seem to be similar to the result of Study of Quality of ANC was carried out in South Ethiopia in August 2020 said quality of antenatal care was significantly associated with residence, educational status[22].
majority of the respondents received these provision comparing with study done in Kenya 2019 showed that more than half of the respondents provided by check of UG, hemoglobin, TT, Iron and anti malarial supplements and less than half of them were provided by U/S[23].
Conclusion:
The study concluded that the age, resident and level of education of the respondents had strong relation with effectiveness of ANC services. The majority of the services provision were provided , There is lack of protocol and guidelines for follow up of female in reproductive age.
References
- Adedoyin-Olowe, M., Gaber, M. M. & Stahl, F., 2014. A survey of data mining techniques for social network analysis. Journal of Data Mining and Digital Humanities
- WHO, UNICEF, UNFPA and The World Bank, Trends in Maternal Mortality: 2000 to 2017, WHO, Geneva, 2019.
- Leontine Alkema-Doris Chou-Daniel Hogan-Sanqian Zhang-Ann-Beth Moller-Alison Gemmill-Doris Fat-Ties Boerma-Marleen Temmerman-Colin Mathers-Lale Say, Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group, The Lancet Published Online November 12, 2015 http://dx.doi.org/10.1016/ S0140-6736(15)00838
- UNICEF, The State of the World’s Children 2021 , UNICEF, New York, 2021.
- Fekede B, G/Mariam A: Antenatalcare services utilization and factors associated in Jimma Town (south west Ethiopia). Ethiop Med J. 2007, 45: 123-133.
- Abou-Zahr CL, Wardlaw T: Antenatalcare in developing countries: Promises, achievements and missed opportunities: An analysis of trends, levels and differentials, 1990-2001. 2003, Geneva, WHO
- Elhassan EM, Mirghani OA, Adam I: High maternal mortality and stillbirth in the Wad Medani Hospital, Central Sudan, 2003-2007. Trop Doct. 2009, 39 (4): 238-9. 10.1258/td.2009.090005
- Ibnouf AH, Vanden Borne HW, Maarse JA: Utilization of antenatal care services by Sudanese women in their reproductive age. Saudi Med J. 2007, 28 (5): 737-43.
- Haggaz A, Ahmed S, Adam I: Use of antenatal care services in Darfur, Sudan. Int J Gynaecol Obstet. 2008, 103 (3): 252-3. 10.1016/j.ijgo.2008.06.010.
- Gezira Initiative for the Safe motherhood &childhood 2005-2010. Omer Ahmed Mirghani, Mohamed Elsanousi, Elhadi Miskeen & Ali Hassan Hessian. Sudan Currency Printing Press
- Global Causes of Maternal Death: A WHO Systematic Analysis. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels JD, et al. Lancet Global Health. 2014;2(6): e323-e333.
- WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division . Maternal mortality: Levels and trends 2000 to 2017. Geneva: 2019. (https://www. who.int/reproductivehealth/publications/maternal- mortality-2000-2017/en/, accessed 17 October 2019).
- [4] Y. Akachi and M. E. Kruk, “Quality of care: measuring aneglected driver of improved health,”Bulletin of the WorldHealth Organization: Policy & Practice, vol. 96, no. 6,pp. 465–472, 2017.
- [5] Health Information and Quality Authority,Guidance onDevelopingKeyPerformance Indicators and Minimum DataSets to Monitor Healthcare Quality: February 2013 (Version1.1), Health Information and Quality Authority, Dublin,Ireland, 2013.
- [6] J. Mainz, “Defining and classifying clinical indicators forquality improvement,”International Journal for Quality inHealth Care, vol. 15, no. 6, pp. 523–530, 2003.
- [7] A. M. Mosadeghrad, “Factors influencing healthcare servicequality,”International Journal of Health Policy and Man-agement, vol. 3, no. 2, pp. 77–89, 2014.
- [8] P. L. Yeoh, K. Hornetz, and M. Dahlui, “Antenatal careutilisation and content between low-risk and high-riskpregnant women,”PLoS ONE, vol. 11, no. 3, Article IDe0152167, 2016.
- M. Nylenna, O. Bjertnaes, I. S. Saunes, and A. K. Lindahl,“What is good quality of health care?”Professions and Pro-fessionalism, vol. 5, no. 1, pp. 1–15, 2015.
- Cormick, G., et al., Interest of pregnant women in the use of SMS (short message service) text messages for the improvement of perinatal and postnatal care. Reprod Health, 2012.
- Abdelmageed E, Bahaeldin H, Nadiah A, Abdelbagi A, Duria R, Ishag A. Maternal and neonatal outcomes of grand multiparity in Khartoum, Sudan. Afr Health Sci. 2022;22(1):164-171. doi:10.4314/ahs.v22i1.21
- Aliya Agency to Expand Educational Opportunities for Their Khalid & Pauline Rose (2023) “We Look Ahead Where his Thoughts Never Reach”: Pakistani Mothers’ Daughters and the Theorisation of Negative Capability, Journal of Human Development and Capabilities, 24:1, 98-117, DOI: 10.1080/19452829.2022.2090524
- Trhas Tadesse Berehe, Lebitsi Maud Modibia, “Assessment of Quality of Antenatal Care Services and Its Determinant Factors in Public Health Facilities of Hossana Town, Hadiya Zone, Southern Ethiopia: A Longitudinal Study”, Advances in Public Health, vol. 2020, Article ID 5436324, 11 pages, 2020. https://doi.org/10.1155/2020/5436324
- Mutai KT, Otieno GO. Utilization of focused antenatal care among expectant women in Murang’a County, Kenya. Pan Afr Med J. 2021;39:23. Published 2021 May 10. doi:10.11604/pamj.2021.39.23.26339
