Hanan A. Khalil1, Aimen M. Rmis2, Salem H. Almadhun3 , Tareg A. Elawaj4, Walid F. Naamat5
1 Department of Information Technology, Faculty of Science and Nature Resources, Al Jafara University; khlilhanan811@yahoo.com
2 Department of Computer Science, Faculty of Science, Alasmarya Islamic University, Zliten, Libya; a.rmis@asmarya.edu.ly
3 Department of Computer, Faculty of Education, Elmergib University, Al Khums, Libya; salem.almadhun@elmergib.edu.ly
4 Department of Computer, Faculty of Education, Elmergib University, Al Khums, Libya; taalawag@elmergib.edu.ly
5 Department of Medical Laboratory, Faculty of Health Science, Alasmarya Islamic University, Zliten, Libya; w.naamat@asmarya.edu.ly
HNSJ, 2023, 4(7); https://doi.org/10.53796/hnsj4716
Published at 01/07/2023 Accepted at 20/06/2023
Abstract
The issue of health is a universal concern that affects individuals of all ages, genders, and social statuses. Access to healthcare is a crucial aspect of modern society and impacts every person throughout their lifetime. The healthcare industry plays a significant role in a country’s Gross National Product (GNP) and is of high public interest and political importance. Individuals are affected by a wide range of diseases, some of which are minor while others require urgent attention. However, providing effective healthcare services remains a significant challenge for developing countries where social services are not as advanced as those in developed countries. The traditional approach to delivering healthcare services has been deemed ineffective. One potential solution to this problem in developing countries is to leverage Information and Communication Technology (ICT) tools, applications, and knowledge, which is commonly referred to as electronic health or e-health. Recent advancements in ICT, such as electronic prescribing, Decision Support Systems (DSS), mobile apps, and Electronic Medical Records (EMR) systems, have become vital components for delivering effective medical services, particularly in developed countries.
The aim of this paper was to investigate the challenges related to the implementation of effective healthcare services in the region. Furthermore, the study sought to identify the determinants that affect the inclination of healthcare service providers towards using e-health technology in healthcare institutions situated in the western region of Libya. The research also highlighted the factors and obstacles that play a crucial role in the successful adoption and execution of e-health technology applications and tools.
Key Words: E-health, Healthcare, Clinical Information, Healthcare Provider, Technology Infrastructure, Patients.
Introduction
Healthcare systems are a complex and critical part of modern society, providing essential medical services to individuals and communities. A healthcare system is defined as “the sum total of all the organizations, institutions, and resources whose primary purpose is to improve health” (World Health Organization, 2000). Healthcare systems are often organized at the national or regional level, with different countries adopting different approaches to healthcare delivery and financing (Topol, E. J., 2019). healthcare is a critical issue that impacts all individuals. Access to high-quality healthcare services is essential for maintaining good health and well-being, and can have a significant impact on an individual’s quality of life (Institute of Medicine (US), 2001). In addition, healthcare costs can be a significant burden for individuals and families, particularly for those who do not have access to affordable healthcare options (Dorsey, E. R., Topol, E. J., & Telemedicine Study Group, 2016).
Healthcare systems play a critical role in addressing these issues by providing access to medical services and resources (World Health Organization, 2021). However, healthcare systems face a range of challenges, including increasing costs, a shortage of healthcare professionals, and disparities in access to care. These challenges require innovative solutions and approaches to ensure that everyone has access to high-quality healthcare services (Fieschi, 2002 & Topcu, 2020).
One approach that has gained increasing attention in recent years is the use of technology, such as telemedicine and digital health tools, to improve healthcare outcomes and increase access to care to (Khalil and Jones, 2007). Telemedicine allows healthcare providers to deliver medical services remotely, which can be particularly useful for individuals living in rural or remote areas. Digital health tools, such as mobile apps and wearable devices, can also help individuals manage their health and wellness by tracking their physical activity, monitoring their vital signs, and providing personalized health advice. The advancement of Information and Communication Technology (ICT) has had a significant impact on the healthcare industry, particularly in developed countries. Electronic prescribing, decision support systems (DSS), mobile applications, and electronic medical records (EMR) are just a few examples of the tools that have become essential for providing efficient medical services (Ludwick & Doucette, 2009).
Overall, healthcare is a critical issue that impacts all individuals, and addressing healthcare challenges requires innovative solutions and approaches. By leveraging technology and other resources, healthcare systems can work towards providing better access to high-quality healthcare services for everyone. A contemporary healthcare system is composed of a complex structure with intricate interactions, integrated with strict regulations as depicted in Figure 1. The healthcare system is made up of various stakeholders, including:
- Healthcare providers: These are the individuals and organizations that provide healthcare services, such as doctors, nurses, and hospitals.
- Consumers: These are the patients who receive healthcare services from healthcare providers.
- Insurance companies: These are the payers who provide financial coverage for healthcare services, either through private insurance plans or government-funded programs.
- Medical drug providers: These are the companies that develop and manufacture pharmaceutical drugs for use in healthcare.
- Diagnostic service providers: These are the organizations that provide diagnostic services such as imaging and laboratory testing.
- Suppliers and vendors: These are the entities that provide goods and services necessary for the operation of healthcare facilities, such as medical equipment and supplies.
Each of these stakeholders interacts with each other in complex ways to provide healthcare services to patients. Additionally, the healthcare system is subject to strict regulations and policies, such as those related to patient privacy and safety, as well as regulations related to the development and approval of new drugs and medical devices.
Overall, the healthcare system is a complex and interconnected network of stakeholders, regulations, and policies, all working together to provide essential healthcare services to individuals and communities.
Figure 1. : illustrates a typical modern healthcare system. [Source: Sneha & Straub, 2017]
Paper Gap
the gap you have identified is the lack of research on the challenges of e-health adoption in Libyan hospitals, specifically in the western region. While the literature has focused on the western part of Libya, it is still important to identify the unique challenges faced in this region. By addressing this gap, your research can contribute to a better understanding of the challenges of e-health adoption in Libyan hospitals and provide insights that could be used to improve healthcare delivery in the region. This could have significant implications for patient care and overall healthcare outcomes in Libya. It’s important to note that addressing a research gap can be challenging, but it also presents an opportunity to make a meaningful contribution to the field.
Paper Motivation
The study aims to investigate the determinants of e-health technology adoption among healthcare service providers in the western region of Libya. This is a critical issue, as the adoption of e-health technology can have significant implications for the delivery of healthcare services in the region. In addition to identifying the determinants of e-health technology adoption, also aims to identify the barriers and critical factors that contribute to the successful implementation and adoption of e-health technology tools and applications. This is important, as the successful implementation of e-health technology requires a range of factors to be considered, including organizational, technical, and cultural factors. Finally, the aims to examine users’ perceptions of e-health technology use. This is a critical aspect, as the sustainability of e-health technology as a solution can only be determined by examining users’ perceptions of its use. Understanding users’ perceptions can help identify areas for improvement and inform strategies for promoting the adoption and sustained use of e-health technology. (Holden & Karsh, 2010).
Paper Scope
This paper aims to investigate the determinants of e-health technology adoption among healthcare service providers in the western region of Libya. The study examines the conditions for effective implementation of e-health technology in primary healthcare, as well as the requirements and difficulties service providers experience in providing e-health services. Specifically, the paper focuses on the perspective of healthcare service providers, as they are the primary actors in determining the current state of technological tools and applications for the given region.
To achieve this, a three-step approach is identified, including a survey of the state of e-health preparedness, a validity test of the findings and conclusion of the e-health readiness assessment, and mapping the results of the validation process onto the constructs of the activity theory framework. The study also determines and examines the variables that influence healthcare professionals’ choices to accept and use e-health tools and apps in low- and middle-income nations, with a particular focus on hospitals located in Libya’s western area.
The paper covers the introduction, study backdrop, and problem, and provides an overview of the entire study, including the research question, goals, scope, and reasons for doing the research. The study’s contribution to the literature is also examined, and it is hoped that the paper’s findings will be helpful to healthcare managers and policymakers in Libya and other developing countries. Overall, this paper provides a comprehensive examination of the determinants of e-health technology adoption in the western region of Libya, with the potential to inform strategies for promoting the adoption and sustained use of e-health technology in developing nations.
Paper Aims and Objectives
The primary goal of this paper is to examine the existing state of healthcare services in the western area of Libya and improve a inclusive framework to assess the level of e-health quickness in hospitals within the region. The paper also aims to examine the challenges associated with establishing efficient healthcare services in the area and creating a technology-based adoption strategy for a contemporary healthcare system, specifically the e-health system.
1. To examine the existing state of healthcare services in the western area of Libya and develop an inclusive framework to assess the level of e-health readiness in hospitals within the region.
2. To identify the challenges associated with establishing efficient healthcare services in the region and create a technology-based adoption strategy for a contemporary healthcare system, specifically the e-health system.
3. To determine the impact of e-health on the organizational and management performance of healthcare institutions.
4. To investigate the current level of e-health adoption and utilization in hospitals within the region and increase knowledge and understanding of e-health advantages in providing sustainable healthcare delivery.
5. To examine the factors that can facilitate or hinder the implementation of e-health in healthcare organizations.
6. To explore the benefits of the e-health system and its support to improving healthcare delivery.
7. To propose a model for an e-health system that hospitals can adopt to measure and manage the capability of their health systems.
8. To identify and recommend strategies to guide hospital management in motivating or stimulating the adoption and utilization of e-health technology.
Overall, the objectives of this paper are to provide a comprehensive analysis of the current state of healthcare services in the western area of Libya, identify the challenges associated with the adoption and implementation of e-health technology, and propose strategies to improve healthcare delivery through the adoption of e-health technology. By achieving these objectives, this paper has the potential to contribute to the advancement of healthcare services in Libya and other developing countries.
Background and Methods
(Pagliari, Detmer, and Singleton 2007) conducted a review of the potential benefits and challenges of electronic personal health records (ePHRs) in healthcare. The authors highlighted the potential benefits of ePHRs, including improved patient empowerment, increased patient involvement in healthcare decision-making, and enhanced communication between patients and healthcare providers. The authors also discussed the potential challenges of implementing ePHRs, such as concerns over privacy and security, data quality and accuracy, and the cost and complexity of implementation. Overall, the study provides insights into the potential benefits and challenges of ePHRs in healthcare and highlights the importance of careful planning and implementation to realize the full potential of this technology. (Cresswell, Bates, and Sheikh 2013) conducted a review of the key considerations for successful implementation and adoption of large-scale health information technology (HIT) systems. The authors identified ten key considerations, including the need for strong leadership and governance, adequate resources and infrastructure, effective change management strategies, and robust evaluation and feedback mechanisms.
(Whitten and Holtz,2008 & Rmis et al.,2020) conducted a study on the utilization of telemedicine by healthcare providers. The authors highlighted the importance of understanding the factors that influence provider utilization of telemedicine, as this technology has the potential to improve access to care, reduce healthcare costs, and enhance healthcare quality. The authors identified several factors that can influence provider utilization, including technical issues, financial considerations, regulatory and legal barriers, and provider attitudes and beliefs about telemedicine. (Gagnon et al. 2011 & Almadhun et al. 2019) conducted a systematic review of the factors that influence the adoption of information and communication technologies (ICTs) by healthcare professionals. The authors identified several categories of factors that can influence ICT adoption, including individual and organizational factors, technical and system-related factors, and external environmental factors. The authors emphasized the importance of understanding the complex interplay of these factors in shaping healthcare professionals’ attitudes and behaviors toward ICT adoption. They also noted that effective strategies to promote ICT adoption must be tailored to the specific needs and contexts of healthcare professionals and organizations. The study provides insights into the challenges and opportunities associated with promoting ICT adoption in healthcare, highlighting the need for a comprehensive and context-specific approach to ICT implementation.
(Liang et al. 2017) conducted a meta-analysis of studies examining the effect of mobile phone interventions for diabetes on glycaemic control. The authors identified 18 randomized controlled trials involving a total of 2,602 patients with diabetes. The meta-analysis found that mobile phone interventions were associated with a significant reduction in HbA1c levels, indicating improved glycaemic control. The authors noted that mobile phone interventions have the potential to improve diabetes management by providing patients with real-time feedback, reminders, and educational resources, as well as facilitating communication between patients and healthcare providers. (Hynes et al. 2016) conducted a study on the use of health information technology (HIT) to advance evidence-based care in the Veterans Affairs Quality Enhancement Research Initiative (VA QUERI) program. The authors highlighted the importance of HIT in supporting the translation of research findings into clinical practice and improving the quality and safety of care. The study identified several key strategies for promoting the adoption and use of HIT in the VA QUERI program, including the development of user-friendly HIT tools, the provision of training and support to healthcare providers, and the use of data and feedback to inform quality improvement efforts. The study provides insights into the potential benefits and challenges of using HIT to advance evidence-based care, highlighting the need for ongoing evaluation and refinement of HIT tools and strategies to support their effective implementation.
Paper Questions
The purpose of the study was to address the following strategic inquiries, which were employed in creating the proposed model for the effective delivery of contemporary healthcare facilities:
What were the strategic inquiries addressed in the study?
Why is it important to understand the current rate of utilization and implementation of e-health knowledge in Libyan hospitals?
What factors were identified as impacting the usage and implementation of e-health applications and systems?
Why is it important for a developing nation like Libya to successfully implement and utilize e-health tools and applications within its hospitals?
How might the proposed model for the effective delivery of contemporary healthcare facilities benefit healthcare organizations in other developing nations?
What are the potential limitations of the study, and how might they be addressed in future research?
Tools and Methodology
The study will employ a mixed-method approach, which means that both quantitative and qualitative data collection techniques will be used. The quantitative data will be collected through a close-ended questionnaire using a survey method, while the qualitative data will be gathered through semi-structured interviews. The survey will provide quantitative data that describes the sample within the selected demographic, while the follow-up semi-structured interviews will be used to validate the research findings and provide in-depth explanations. The purpose of this methodology is to arrive at a comprehensive conclusion by utilizing both quantitative and qualitative data. (Venkatesh et al. 2013 & Rmis et al. 2021).
The term “completeness” is used to describe the extent of data collected. The survey’s target population will be healthcare professionals from hospitals in the western region of Libya. The hospitals will be selected using a cluster random selection technique, while the survey participants will be chosen using a simple random sample procedure.
The Statistical Package for the Social Sciences (SPSS version 20.0) will be used to evaluate the obtained data. Several statistical tests will be conducted using the SPSS software, including frequency distribution tests for participant demographic data analysis, reliability tests to determine the measuring instrument’s Cronbach’s Alpha value, correlation coefficient analysis to determine the relationship between independent and dependent variables, and linear regression analysis to determine how the independent variables influence the dependent variables. The purpose of the frequency distribution tests is to describe the characteristics of the sample population, while the reliability tests will assess the consistency and accuracy of the measuring instrument. The correlation coefficient analysis will determine the strength and direction of the relationship between the independent and dependent variables, while the linear regression analysis will determine the extent to which the independent variables influence the dependent variables. ( Almadhun et al. 2021).
Is there a correlation between the dependent variables of attitudes toward e-health, perceived usefulness, and intentions to use e-health, with the external factors of technical infrastructures, information sharing, staff IT experience, and security concerns?
Based on these research questions, the following hypotheses were formulated:
H1: Attitudes regarding e-health and intentions to use it are positively correlated.
H2: The perceived usefulness of e-health and usage intentions are positively correlated.
H3: Information sharing and plans to use e-health are positively correlated.
H4: Staff IT experience and e-health use intentions are positively correlated.
H5: Technical infrastructures and e-health use intentions are positively correlated.
H6: There is an association between e-health usage intentions and security worries.
Paper Model and Design
This research utilizes a cross-sectional design to examine the factors that impede the adoption and implementation of e-health frameworks and technologies by healthcare workers and organizations in developing countries such as Libya. The study employs a quantitative methodology, and a survey design was deemed the most appropriate approach.
The Technology Acceptance Model (TAM) is utilized in this research as a well-established framework for understanding the factors that hinder healthcare professionals and organizations from adopting and implementing new technology. However, an extended version of TAM is proposed and employed in this study to analyze the related factors that promote the approval of e-health technology by healthcare organizations and professionals.
To enhance the predictive power of TAM, new variables such as security measures, technical infrastructures, information sharing, and staff IT knowledge are included in the proposed theoretical model. The survey method is employed in this research to collect data from various relevant hospitals in Libya using closed-ended questionnaires.
The survey method is selected for its efficacy in obtaining significant data from a vast population, its affordability, and its capacity to cover a broad population within a restricted time frame. This research serves as a notable pilot study for examining the factors that impede the adoption of e-health frameworks and technologies in developing countries such as Libya.
4.1 Population and Sample
The capital city of Libya, Tripoli, has over 30 hospitals and clinics, comprising both private and public healthcare facilities. These thirty hospitals and clinics were included as the population for this study. The study focuses on relevant healthcare professionals, such as doctors, nurses, healthcare professionals, matrons, laboratory officials, and health directors, from different hospitals and clinics for the purpose of this research.
4.2 DatasCollection andsInstrument
Various methods can be utilized to gather information in a research study aimed at addressing a specific problem. In this research, a quantitative survey method was employed, as previously mentioned, through the use of closed-ended questionnaires to gather data from fifteen (15) hospitals selected from the capital city of Libya.
- Questionnaire Format and Contents
This research utilized a structured questionnaire consisting of closed-ended questions with a set of predefined responses. To simplify the survey process and data analysis, a 5-point Likert scale was employed to rate the survey questions, with 1 indicating ‘strongly agree,’ 2 indicating ‘agree,’ 3 indicating ‘neutral,’ 4 indicating ‘disagree,’ and 5 indicating ‘strongly disagree.’ To measure the participants’ IT literacy and experience level, the following scale was utilized: none (indicating no IT literacy), low (indicating little IT literacy), fair (indicating average IT literacy), and high (indicating sufficient IT literacy).
4.3 Data Collection Procedures.
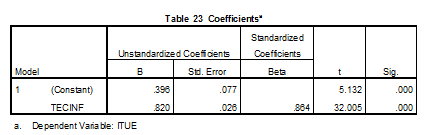
The data collection process adhered to ethical principles, and the questionnaire was developed based on the guiding principles prescribed by Ssegawa(2003). A total of 450 questionnaires were distributed, and 380 copies were collected. However, only 350 questionnaires were considered for further analysis, as 30 questionnaires had incomplete or blank responses. The collected data was analyzed using SPSS software. Table 1 presents the response rate achieved in this study:
Table 1:The Responses Rate of the Questionnaires.
Data Presentation and Analysis
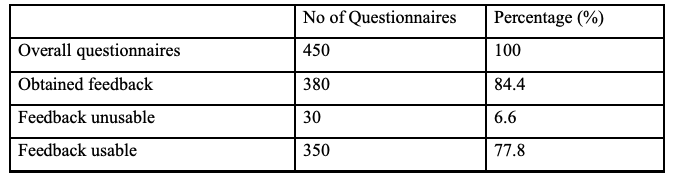
Respondents Sex Distribution:
The analysis of Table 2 revealed that 62.9%, or 220 respondents, were male, while 37.1%, or 130 respondents, were female. As it is common in developing countries, there is gender inequality in employment opportunities. This finding aligns with Dormekpor’s (2015) research that showed gender inequality in employment opportunities, especially in emerging nations. However, this gender imbalance did not affect the results of this study.
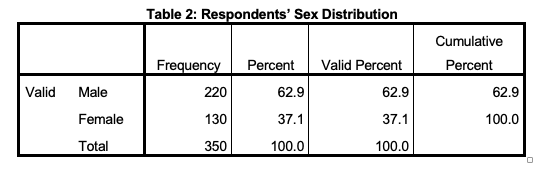
Respondents Position/Profession in the Hospital:
 |
The above table indicates that 2.9%, or 10 respondents, were Medical Directors, 30.9%, or 108 respondents, were Doctors, 23.4%, or 82 respondents, were Nurses, 21.7%, or 76 respondents, were Radiologists, and 21.1%, or 74 respondents, were Laboratory Technologists. This diverse representation of healthcare professionals provides a well-rounded perspective and generalizability of the study results. Previous research has focused solely on doctors, ignoring other healthcare professionals, potentially leading to biased results. Therefore, this study takes a step forward by including a broader range of health professionals in the study.
Years of Experience in the Position of Respondents:
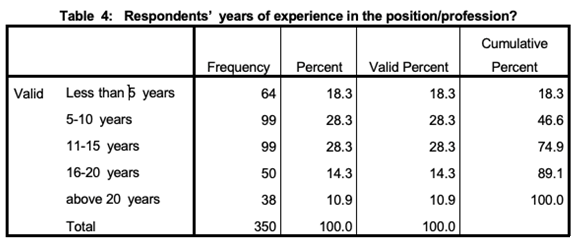
Table 4 indicates that 18.3% of all respondents, or 64 individuals, had less than 5 years of professional experience, 28.3% or 99 individuals had 5 to 10 years of professional experience, 28.3% or 99 individuals had 11 to 15 years of professional experience, 14.3% or 50 individuals had 16 to 20 years of professional experience, and 10.9% or 38 individuals had over 20 years of professional experience. It is worth noting that the findings of Simon et al. (2007) and Or & Karsh (2009) suggest that individuals who use new technologies in an organization are typically younger and possess higher IT skills than the general population.
The IT literacy and experience level of the participants:
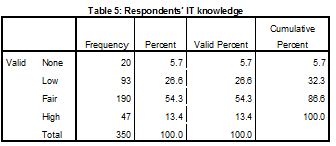
Table 5’s data reveals the respondents’ level of IT experience and knowledge. 20 respondents, or 5.7% of the total, had no prior IT knowledge or experience. In contrast, 93 respondents, or 26.6%, claimed to have minimal familiarity with and experience with IT. 190 respondents, or 54.3%, reported to have an adequate amount of IT literacy and skill, proving their ability to operate a computer for basic tasks like sending emails and accessing the internet. Finally, it was discovered that 47 respondents, or 13.4%, had substantial IT knowledge and skill.
Evaluation of the proposed hypotheses and a discourse of the obtained results:
- Hypothesis 1:
H1: Attitudes regarding e-health and intentions to use it are positively correlated.
In order to test this hypothesis, a regression analysis was performed, and the preceding tables contain proof of what was discovered:
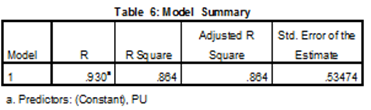
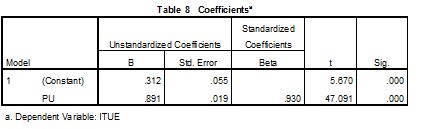
The model summary’s findings, which were used to assess the independent variable’s (perceived usefulness) predictive ability to explain and forecast the dependent variable (intention. to use), are shown in Table 6. A high level of correlation between “impression of utility” and “intention. to use” is shown in the table, with a correlation coefficient of 0.930, showing a strong linear link between the values of the dependent variable that were actually observed and those that were expected. The coefficient of determination (R square) is 0.864, indicating that 86.4% of the variation in the dependent variable (intention. to use) was explained by the independent variable (perceived usefulness).
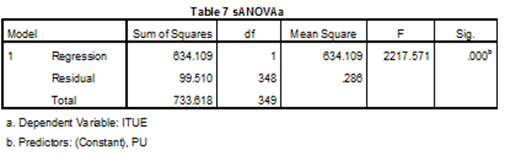
The ANOVA score, which was used to figure out the importance of the influence of perceived usefulness on the intention. to use e-Health, is shown in Table 7. The analysis of variance (ANOVA) result table illustrates a P-value of 0.000, showing that the model was significantly affected by perceived usefulness. The fact that the P-value is less than the alpha value of 0.01 suggests that there is significant impact of estimated utility on the decision to use eHealth.
According to Table 8’s correlations table, the “Intention. to use” is clarified by 0.312—a constant—and 0.891—”perceived usefulness” The regression equation ITUE.= 0.312. + 0.891. PU is used to assess the impact of “perceived usefulness” on “intention. to use” The model predicts that, if other parameters stay constant, for every unit change in “perceived usefulness,” there will be 0.891 unit changes in “Intention. to use.”
In therefore, the findings support the prediction that there is a positive correlation between perceived usefulness and the intention to adopt electronic health records.
- Hypothesis 2:
H2: The perceived usefulness of e-health and usage intentions are positively correlated.
Regression analysis was executed out to evaluate this assumption, and the tables which followed reflect how it turned out:
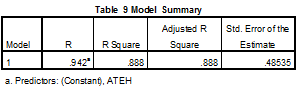
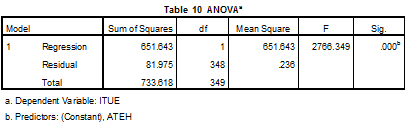
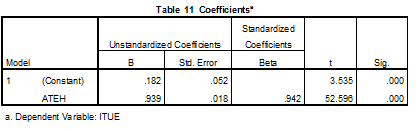
The model summary’s findings are shown in Table 9, and they were used to assess how well the independent variable (attitude toward eHealth) could explain and predict the dependent variable (Intention. to use). The table demonstrates a strong linear link between the observed and anticipate.d values of the dependent variable, with a positive correlation between “attitude towards eHealth” and “Intention. to use,” as indicated by the correlation coefficient of 0.942. The coefficient of determination (R square) is 0.888, indicating that 88.8% of the variation in the dependent variable (intention. for use) was explained by the independent variable (attitude toward eHealth).
The significance of the relationship between attitude toward e-health and intention to utilize e-health is shown in Table 10 by the ANOVA score. The ANOVA table shows a P-value of 0.000, indicating that the model’s attitude toward eHealth was significantly impacted. The fact that the P-value is less than the alpha value of 0.01 suggests that there is a strong relationship between attitude toward e-health and the desire to utilize it.
According to Table 11’s coefficients table, the “Intention. to use” is described by 0.182, which is a fixed value, and 0.939 of “attitude toward eHealth.” ITUE.= 0.182. + 0.939 ATEH. is the regression equation used to assess the impact of “attitude towards eHealth” on “Intention. to use.” According to the model, when other parameters stay constant, there will be 0.939 units of change in “Intention. to use” for every unit change in “attitude towards eHealth.”
The hypothesis presenting a favourable association between attitude toward eHealth and the desire to utilize eHealth is accepted, we may conclude based on the data.
- Hypothesis 3
H3: Information sharing and plans to use e-health are positively correlated.
To investigate this hypothesis, a regression analysis was conducted, and the resulting tables describe the way it came about:
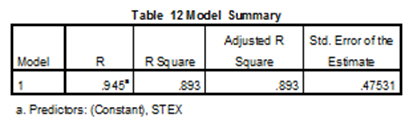
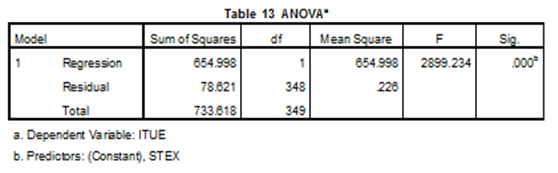
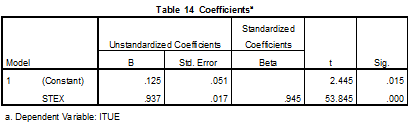
The model summary’s findings, which assessed the independent variable (Staff IT Experience)’s capacity to explain and predict the dependent variable (Intention. to use), are displayed in Table 12. The table illustrates a strong linear relationship between “staff IT experience” and “Intention. to use,” with a correlation coefficient of 0.945, indicating a positive association between the actual and anticipated values of the dependent variable. With a degree of determination (R square) of 0.893, the uncorrelated variable (staff IT experience) explained 89.3% of the variance in the dependent variable (intention to utilize).
The analysis of variance (ANOVA) scores, which was used to assess the significance of the effect of staff IT experience on the intention to utilize e-Health, appears within Table 13 beneath. The P-value in the ANOVA table is 0.000, demonstrating that the hypothesis was significantly influenced by the crew members’ IT experience. The fact that the P-value is less below the alpha value of 0.01 implies that there is a strong relationship between staff IT experience and intention to adopt e-Health.
According to Table 14’s coefficients table, the “Intention. to use” is described by a constant 0.125 and a factor called “staff IT experience” of 0.937. ITUE.= 0.125. + 0.937 STEX. is the regression equation used to assess the impact of “staff IT experience” on “Intention. to use.” According to the model, while other parameters stay constant, there will be 0.937 units of change in “Intention. to use” for every unit change in “staff IT experience.”
In light of the findings, the hypothesis positing a favourable association between staff IT experience and the desire to utilize e-Health is accepted.
- Hypothesis 4
H4: Staff IT experience and e-health use intentions are positively correlated.
In order to test this hypothesis, an examination of regression was done and the after tables show how it came about:
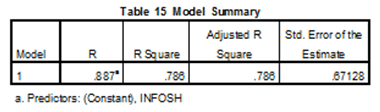
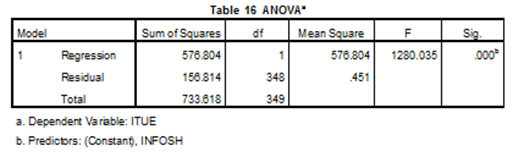
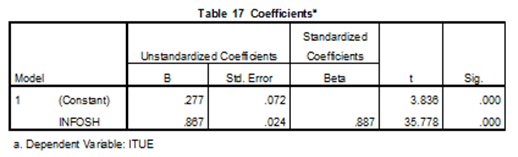
The purpose of the study was to investigate the impact of information sharing on the Intention. to use e-Health. The results are presented in three tables. Table 15. provides a model summary showing a positive correlation between information sharing and Intention. to use, with a correlation coefficient of 0.887 and a coefficient of determination of 0.786. This demonstrates that data interchange was responsible for 78.6% of the difference in e-Health adoption intentions.
The finding from the ANOVA can be found in Table 16, and it suggests that information sharing had a substantial influence on the statistical model. The P value of 0.000 is smaller than the alpha value of 0.01, demonstrating that information sharing has a significant impact on people’s motivation to use e-Health..
The coefficients for the model are displayed in Table 17. The desire to utilize e-Health is explained by the constant (0.277) and information sharing (0.867). ITUE.= 0.277. + 0.867. INFOSH is the regression equation used to examine the impact of information sharing on Intention. to use. Keeping all other variables fixed, this suggests that for every unit change in information sharing, there is a 0.867 unit change in the desire to utilize e-Health.
The study’s findings support the notion that data exchange and the intention to adopt e-Health are positively correlated. The results imply that expanding information exchange can strengthen the desire to utilize e-Health.
- Hypothesis 5
H5: Technical infrastructures and e-health use intentions are positively correlated.
A regression analysis was carried out to evaluate this hypothesis and the after tables show how it came about:
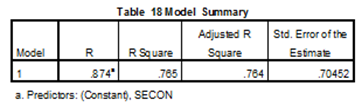
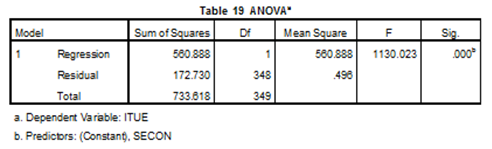
The purpose of the study was to ascertain how people’s intentions to use e-Health were impacted by security concerns. The results are displayed in three tables. Table 18 presents. a summary of the model and indicates the positive relationship between security concern and Intention. to use, with a correlation value of 0.874 and a coefficient of determination of 0.765. This shows that security concerns accounted for 76.5% of the change in the Intention. to use e-Health.
Security concerns had a considerable influence on the model, as evidenced by the ANOVA score in Table 19 of the results. The P value of 0.000 is smaller than the alpha value of 0.01 and shows that security concerns have a significant impact on people’s willingness. to use e-Health.
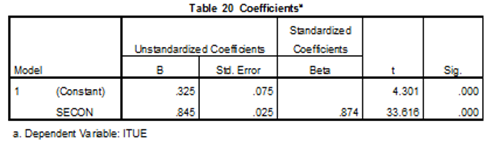
Table 20 lists the coefficients for the model. The choice to use e-Health is justified by ongoing (0.325) and security-related (0.845) concerns. The regression equation used to study the effect of security concern on Intention. to use is ITUE.= 0.325 + 0.845 SECON. As a result, every unit change in security concern results in a 0.845 unit change in the desire to adopt e-Health while all other factors remain constant.
In its conclusion, the study finds a correlation between security worries and the willingness to use e-Health. The study found that resolving security problems increased consumers’ inclinations to adopt e-Health.
- Hypothesis 6
H6: There is an association between e-health usage intentions and security worries.
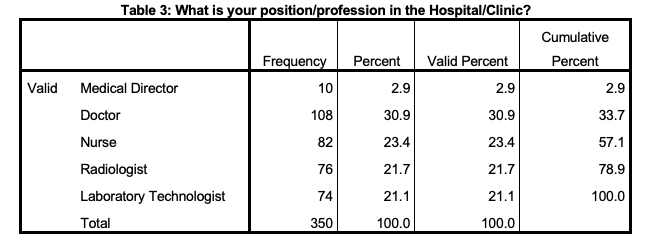
Regression analysis was used to evaluate this hypothesis and the following tables provide evidence of the result:
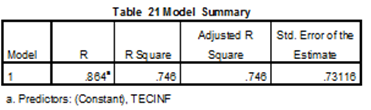
The study’s goal was to investigate the connection between technological capabilities and E-Health adoption intentions. Three tables with the results are shown. The model summary’s findings are shown in Table 21, which examined the technological infrastructure’s capacity to explain and forecast e-Health use intentions. With correlation coefficients of 0.864 and coefficients of determination (R square) of 0.746, the table shows a favorable association between technological infrastructure and desire to use. This indicates that 74.6% of the change in the desire to adopt e-Health was due to technological infrastructure.
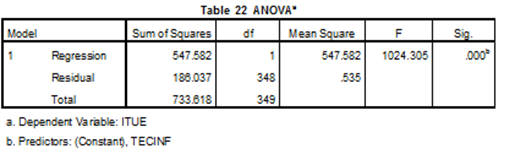
The ANOVA score, which was used to determine the importance of the impact of technological infrastructure on the intention to utilize e-Health, is shown in Table 22. The table’s P value of 0.000, which is lower than the alpha value of 0.01, demonstrates that the model was significantly impacted by technological infrastructure.
According to Table 23, which contains the model’s coefficients, the constant (0.396) and technological infrastructure (0.820) account for the intention to adopt e-Health. ITUE= 0.396 + 0.820 TECINF is the regression equation used to examine the relationship between technical infrastructure and Intention. to use. Accordingly, while maintaining all other variables equal, every unit change in technological infrastructure results in a 0.820 unit change in the intention to utilize e-Health.
The study supports the idea that there is a link between the availability of technological infrastructure and the intention to employ e-Health. According to the research, enhancing technological infrastructure can increase user intent to utilize e-Health.
Conclusion
The crucial objective of this research is to explore the barriers to adoption and implementation technology of e-health and bases in health foundations in developing countries, with a specific focus on Libya. The study aims to investigate the perceptions of healthcare practitioners in Libya regarding critical factors that prevent the adoption of these technologies. The ultimate objective is to aid in the adoption of long-term e-health frameworks and technology in Libyan healthcare facilities, which can result in the provision of high-quality healthcare services in the nation. The results of this study can serve as a guide for other emerging countries.
Additionally, more study is required to build health applications in Libya that may be used to monitor individuals with unusual or persistent disorders. These programs can also make it easier for nations to exchange medical knowledge and advancements, and they can help international health councils react more promptly to public health emergencies.
References
Almadhun, Salem Husein, Salem M Aldeep, Aimen M Rmis, and Khairia A Amer. “Examination of 4G (LTE) Wireless Network.” El tarbawe journal 19, no. 1 (July 2021): 285–94. https://doi.org/http://dspace.elmergib.edu.ly/xmlui/handle/123456789/1119.
Almadhun, Salem, Mehmet TOYCAN, and Ahmet ADALIER. “VB2ALGO: An Educational Reverse Engineering Tool to Enhance High School Students’ Learning Capacities in Programming.” Revista de Cercetare si Interventie Sociala 67 (2019): 67–87. https://doi.org/10.33788/rcis.67.5.
Berner, E. S., Detmer, D. E., & Simborg, D. (2005). Will the wave finally break? A brief view of the adoption of electronic medical records in the United States. Journal of the American Medical Informatics Association. 12(1), 3-7. DOI: 10.1197/jamia.M1664
Brandner, R., van der Haak, M., Hartmann, M., Haux, R., & Schmücker, P., (2002). Electronic .
Cresswell, K. M., Bates, D. W., & Sheikh, A. (2013). Ten key considerations for the successful implementation and adoption of large-scale health information technology. Journal of the American Medical Informatics Association, 20(e1), e9-e13.
Dorsey, E. R., Topol, E. J., & Telemedicine Study Group. (2016). State of telehealth. New England Journal of Medicine, 375(2), 154-161.
Eysenbach, G. (2001). What is e-health? Journal of Medical Internet Research, 3(2), e20 www.jmir.org/2001/2/e20.
Fieschi, M. (2002), Information technology is changing the way society sees health care delivery. International Journal of Medical Informatics, 66, 85-93.
Gagnon, M. P., Desmartis, M., Labrecque, M., Car, J., Pagliari, C., Pluye, P., & Turcot, L. (2011). Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. Journal of medical systems, 36(1), 241-277.
Holden, R. J., & Karsh, B. (2010). The technology acceptance model: its past and its future in healthcare. Journal of Biomedical Informatics, 43, 159-172.
Hynes, D. M., Weddle, T., Smith, N., Whittier, E., Atkins, D., Francis, J., … & Krucoff, M. W. (2016). Use of health information technology to advance evidence-based care: lessons from the VA QUERI program. Journal of general internal medicine, 31(Suppl 1), 1-8.
Ilie, V., Van Slyke, C., Parikh, M. A., & Courtney, J. F. (2009). Paper versus electronic medical records: the effects of access on physicians’ decisions to use complex information technologies. Decision Sciences, 40(2), 213-241. DOI: 10.1111/j.1540-5915.2009.00227.x
Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK222274/
Khalil, M. M., & Jones, R. (2007). Electronic Health Services An Introduction to Theory and Application. Libyan Journal of Medicine, 2(4), 202-210.
Liang, X., Wang, Q., Yang, X., Cao, J., Chen, J., Mo, X., & Huang, J. (2017). Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabetic medicine, 34(6), 802-813.
Ludwick, D. A., & Doucette, J. (2009). Adopting electronic medical records in primary care: Lessons learned from health information systems implementation experience in seven countries. International Journal of Medical Informatics, 78, 22-31.
Oh, H., Rizo, C., Enkin, M., & Jadad, A. (2005). What is eHealth (3): a systematic review of published definitions. Journal of medical Internet research, 7(1).
Pagliari, C., Detmer, D., & Singleton, P. (2007). Potential of electronic personal health records. BMJ: British Medical Journal, 335(7615), 330-333.
Patel, M. S., Asch, D. A., & Volpp, K. G. (2018). Wearable devices as facilitators, not drivers, of health behavior change. JAMA, 319(3), 247-248.
Rmis, A. Alkazagli, M. Alloush. O. Almadhun, Salem. (2021). Sentiment Classification Using Three Machine Learning Models. Vol. 34 No. 1, June.
Rmis, Aimen & Topcu, Ahmet. (2020). Evaluating Riak Key Value Cluster for Big Data. Tehnicki vjesnik – Technical Gazette. 27. 10.17559/TV-20180916120558.
Sesselberg, T. S., Cantrill, J. A., Gray, N. J., Klein, J. D., Noyce, P. R. (2005). The Internet: a window on adolescent health literacy. J Adolesc Health. 37(3):243.
Sneha, S, & Straub, D. (2017). E-health: Value proposition and technologies enabling collaborative healthcare. In Proceedings of the 50th Hawaii International Conference on System Sciences (HICSS 2017). 920-929.
Sneha, S., & Varshney U. (2009). Enabling ubiquitous patient monitoring: Model, decision protocols, opportunities and challenges. Decision Support Systems, 46(3): 606-619. DOI: 10.1016/j.dss.2008.11.014.
Steininger, K., & Stiglbauer, B. (2015). EHR acceptance among Austrian resident doctors. Health Policy and Technology, 4(2), 121-130. DOI: 10.1016/j.hlpt.2015.02.003.
Topcu, Ahmet & Rmis, Aimen. (2020). Analysis and Evaluation of the Riak Cluster Environment in Distributed Databases. Computer Standards & Interfaces. 72. 103452. 10.1016/j.csi.2020.103452.
Topol, E. J. (2019). High-performance medicine: the convergence of human and artificial intelligence. Nature Medicine, 25(1), 44-56.
Venkatesh, V., Brown, S. A., & Bala, H. (2013). Bridging the qualitative-quantitative divide: guidelines for conducting mixed methods research in information systems. MIS Quarterly, X(X), 1-34.
Whitten, P., & Holtz, B. (2008). Provider utilization of telemedicine: the elephant in the room. Telemedicine and e-Health, 14(9), 995-997.
World Health Organization. (2000). The World Health Report 2000. Health systems: improving performance. Geneva: World Health Organization.
World Health Organization. (2021). Digital health. Retrieved from https://www.who.int/health-topics/digital-health#tab=tab_1