Prevalence of Anaemia in Type 2 Diabetes Mellitus for chronic kidney disease patients at the Alkhums Kidney Services Center – Libya
Amer mohamed A. abdurahman1, Mohmmed Ismail Abosalah2, Abdullah Ali Aboughuffah3, Walid Faraj Naamat4
1 Department of medical laboratories, Faculty of medical technique, Elmergib University, Al Khums, Libya;
amabdurahman@elmergib.edu.ly
2 Department of Health Management, Faculty of health sciences, Alasmarya Islamic university Email:
m.abosalah@asmarya.edu.ly
3 Department of public health, Faculty of health sciences, Alasmarya Islamic university Email:
ahmaddd256@asmarya.edu.ly
4 Department of Medical Laboratory, Faculty of health sciences, Alasmarya Islamic university. Email:
w.naamat@asmarya.edu.ly
HNSJ, 2024, 5(7); https://doi.org/10.53796/hnsj57/28
Published at 01/07/2024 Accepted at 05/06/2024
Abstract
The presence of anemia in people with diabetes mellitus type 2. (T2DM) is a common and significant finding, representing a substantial and often unrecognized burden. This study aimed to investigate the prevalence and characteristics of anaemia in T2DM patients, with an emphasis on the roles that iron deficiency and persistent inflammation may play. The differentiation between these factors is particularly challenging in countries like Libya, where iron deficiency is prevalent. Additionally, the presence of other underlying causes of anaemia further complicates the interpretation. The study identified renal disease, including renal impairment and albuminuria, as significant risk factors for anaemia in T2DM patients. The results indicated that approximately two-thirds of T2DM patients in the study were anaemic, with a predominance of microcytic hypochromic anaemia. Furthermore, when the prevalence of chronic renal disease and albuminuria rose among T2DM individuals, the severity of anaemia also escalated. These findings highlight the importance of early detection and management of anaemia in T2DM, particularly in patients with renal complications.
Key Words: Diabetes. , CKD, Creatinine, Anaemia
INTRODUCTION.
Diabetes is a chronic illness that has existed since 1500 BC., the period of the Egyptian papyrus. Renowned physicians Charak and Sushruta reported a strange symptom in certain patients: sweet pee (called Madhumeh or honey urine) combined with polyuria, or frequent urination.1
Hyperglycemia, or high blood glucose, is a hallmark of a series of metabolic illnesses collectively referred to as diabetes mellitus. The burden that this metabolic dysregulation places on people with diabetes and the healthcare system as a whole is immense, since it causes a variety of pathological alterations in many organ systems2.
The main cause of end-stage renal disease in the US is diabetes mellitus. In addition, diabetes mellitus is becoming increasingly commonplace worldwide and will soon overtake all other causes of illness and death. Globally, the prevalence of diabetes has increased significantly throughout the last 20 years.3
Type 2 diabetes is predicted to develop more often than type 1 diabetes despite both types of the disease being on the rise. This is because type 2 diabetes is associated with higher rates of obesity and lower levels of physical activity. The International Diabetes Forum estimates that over 194 million people worldwide have diabetes now, and by 2025, this figure will have doubled.4
An additional health burden for those with diabetes mellitus is anemia, a disorder that is becoming better recognized. When compared to individuals with comparable renal impairment and iron levels in the general population, the prevalence of anemia in diabetes patients is two to three times greater. According to research, having diabetes and anemia together may raise your risk of stroke, cardiovascular disease, and diabetic retinopathy. Furthermore, persons who have both diabetes and anemia have a higher chance of dying young than those who only have diabetes. This is especially true for diabetic anemia patients who simultaneously have heart failure or renal dysfunction.6, 10
METHODS
The primary goal of the study, which was conducted at the Kidney Services Center – Alkhums in Libya, was to ascertain the kinds and prevalence of anemia among individuals with type 2 Diabetes Mellitus.12
For the study, sample of 100 individuals with T2DM who were being treated in the General Medicine departments indoors and outdoors were chosen. All patients got a comprehensive clinical examination, a full medical history, and a number of investigations after providing their informed written permission.16
The Kidney Services Center – Alkhums in Libya’s computerized central laboratory was the site of the studies performed on each participant.14, 15
Hemoglobin levels were measured as part of a full blood count in these studies.
To evaluate their health, the patients with diabetes and anemia conducted a number of tests. These tests included a kidney function test, routine and microscopic urine analysis, ESR, blood sugar measurement, peripheral smear analysis to identify the type of anemia, reticulocyte count, creatinine clearance measurement, and routine and microscopic stool examination for occult blood. Further studies, such the HBA1c test, were carried out if required. The Cockcroft-Gault equation was utilized to determine the creatinine clearance in these individuals, accounting for variables including age, weight, and serum creatinine levels.13, 14
Statistical analysis
To understand and examine the collected data, statistical analysis was done. An unpaired student t-test was used to determine the mean difference between diabetes patients who were anemic and those who were not. Furthermore, Pearson correlation was used to establish the relationship between the haemoglobin level and the albumin-creatinine ratio, which is a measure of renal impairment. The data was examined using statistical software, including SPSS 10 and Microsoft Excel 2010.11
RESULTS.
All analyzed cases in this research came from the outpatient department and various medical wards of the Kidney Services Center – Alkhums in Libya. The following findings were noted:
Table 1: The frequency of anemia in individuals with type 2 diabetes.
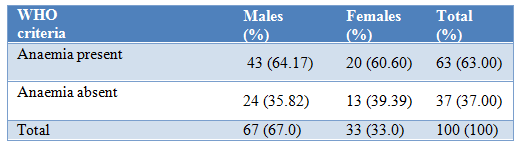
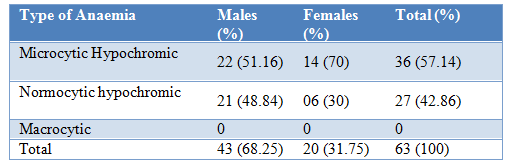
Table 2: Anaemia types Distribution.
Anaemia was discovered in 63.00% of the 100 individuals with Type 2 diabetic Mellitus. 31.75% of these anemic patients were female, and 68.25% of them were male.
Fourteen of the sixty-six anemic individuals had normocytic hypochromic anemia, and fifty-seven percent had microcytic hypochromic anemia. Macrocytic anemia did not affect any of the individuals.
According to Table 2, the most prevalent cause of anemia in both males (51.16%) and the females’ percentage was (70%) and all of them are microcytic hypochromic anemia.
Moreover, Table 3 demonstrates that the majority of anemic individuals (88.88%) had a creatinine clearance ranging from 31 to 60 milliliters per minute. Conversely, The majority of those who did not have anemia (48.78%) had a creatinine clearance between 61 and 90 ml/min. Interestingly, patients with a creatinine clearance of less than 30 ml/min had a 100% incidence of anemia, but patients with a clearance of more than 90 ml/min had a prevalence of just 18.75%.
Table 3: Renal function assessment in a group of patients diagnosed with type 2 diabetes.
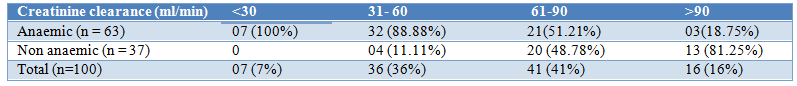
Table 4: Haemoglobin level VS albuminuria.
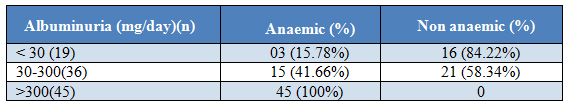
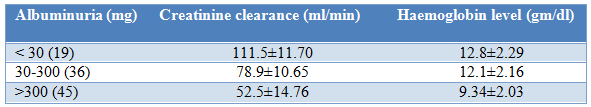
Table 5: Albuminuria VS creatinine and haemoglobin.
Only three patients (4.77%) of the 63 anemic individuals had albuminuria values < 30 mg/day, whereas 60 patients (95.23%) had levels > 30 mg/day.
Twenty-one of the non-anemic individuals had albuminuria levels > 30 mg/day, whereas only 16 of them had values < 30 mg/day. It is noteworthy that, as Table 4 illustrates, the prevalence of anemia rose in tandem with the amount of albuminuria.
The average creatinine clearance and mean HB level for patients with normoalbuminuria (urinary albumin less than 30 mg/day) were 111.5±11.70 and 12.8±2.29.
For those patients with macroalbuminuria (urinary albumin >300 mg/day) and microalbuminuria (urinary albumin 30-300 mg/day), the mean creatinine clearance was 52.5±14.76 ml/min, respectively. According to Table 5, the mean HB level was 9.34±2.03 gm/dl for patients with macroalbuminuria and 12.1±2.16 gm/dl for patients’ people with microalbuminuria.
DISCUSSION
Incidence of anemia.
Of the one hundred patients included in this study, sixty-three (63%) were determined to be anemic, and the remaining thirty-seven (37%), not anemic. However, a different study by Ezenwaka CE et al. with 155 participants suffering from type 2 diabetes mellitus discovered that 72 patients (46.45%) and 83 patients (53.54%) were anemic. In a different study by Cawood TJ et al., out of 270 patients, only 34 people (12.29%) were found to be anemic. The higher incidence of anemia observed in this study is probably due to factors such as poverty-related malnutrition, rising incidence and degree of infections and chronic diseases, limited access to healthcare, and lack of knowledge about a balanced diet. Twenty patients (31.74%) were female and 43 patients (68.25%) were male among the 63 anemic patients in this study. Likewise, in the research carried out by Cawood TJ et al., 19 people (55.88%) and 15 persons (44.11%) of the 34 anemic patients were male.7
Types of anaemia
Of the sixty-three anemic individuals that were part of this study, normocytic normochromic anemia affected thirty-seven (42.86%), whereas microcytic hypochromic anemia affected thirty-six (57.14%). It is noteworthy that microcytic hypochromic anemia was identified in the majority of anemic individuals, notably in 22 (34.92%) males and 14 (22.22%) females. This result is in contrast to a prior research by Cawood TJ et al. that found that normocytic anemia was present in 85% of anemic individuals.11
14.3% of patients had microcytic anemia and 87.5% of patients had normocytic anemia, according to a different research by Yun YS et al. The higher incidence of microcytic hypochromic anemia in this study can be linked to variables including poverty, malnourishment, and a higher frequency of female pregnancy. It is also interesting that the majority of patients with any kind of anemia were in the 51–60 age range.
Anaemia was identified in 32 individuals (50.79%) out of the total number in the 51–60 age range. Microcytic hypochromic anemia was seen in 14 (43.75%) of them, whereas normocytic hypochromic anemia was present in 18 (56.25%). Macrocytic anemia was absent in all of the individuals. In this investigation, the length of type 2 diabetes mellitus was not shown to be significantly correlated with the kind of anemia.10
Research indicates that those with type 2 diabetes mellitus between 16 and 20 years had the highest frequency of hypochromic anemia, both normocytic and microcytic. Nevertheless, there was no discernible link found between the particular form of anemia and its symptoms. Across all forms of anemia, symptoms like weakness, giddiness, and anorexia were more frequently reported than symptoms like palpitations, tinnitus, and dyspnea. In a similar vein, all anemia patients, regardless of kind, had the pallor symptom.9
Creatinine. clearance
Anemia prevalence decreased in this research as creatinine clearance rose. For every 100 people with a type 2 diabetes diagnoses, 100% of them had anemia if their creatinine clearance was less than 30 milliliters per minute, but only 18.75% of them had the same level of prevalence. Patients with diabetes, both male and female, likewise showed same tendency. Thomas MC et al. found that patients with type 2 diabetes mellitus who had a creatinine clearance of < 60 ml/min were twice as likely to have anemia as those who had a clearance of >90 ml/min. Similarly, patients with diabetes who had a clearance of 60 to 90 ml/min were twice as likely to have anemia. These results were in line with that study.5
In the current investigation, 51.21% of diabetic individuals with a creatinine clearance of greater than 60 ml/min had anemia. However, 72% of patients with a creatinine clearance of greater than 60 ml/min were anemic, according to a research by Cawood TJ ET al.9,These findings suggest that the causes of anemia in type 2 diabetes mellitus extend beyond diabetic nephropathy. Diabetic patients with anaemia had significantly worse clearance of creatinine (67.1±3.0 ml/min) compared to those without diabetes (57.9±5.4 ml/min) (p<0.001), based on another study by Ezenwaka CE et al.8
Albuminuria
We found that there was a relationship between anemia and albuminuria levels in this study. Just 3 out of 19 patients (15.78%) with normoalbuminuria were determined to be anemic. Nevertheless, the frequency of anemia was 100% in individuals with macroalbuminuria and 41.66% in those with microalbuminuria. These results are consistent with a research by Thomas MC et al. that produced conclusions that were comparable.5
Albumin-creatinine ratio
The results of the study showed that the albumin creatinine ratio and hemoglobin level were negatively correlated. Therefore, the Hb level dropped as the albumin creatinine ratio rose. This discovery is consistent with the research that Cawood TJ et al. published.9
CONCLUSION
As a result, it can be concluded that anemia represents a substantial and sometimes disregarded burden and is a common finding in people with type 2 diabetes mellitus. A combination of iron shortage and persistent inflammation from the illness itself can be the cause of anemia in these people. Differentiating between these two variables is especially difficult in a nation like Libya where iron shortage is common. Furthermore, the coexistence of other conditions that may be contributing to anemia may make its interpretation more difficult. Anaemia is more common in patients with renal disease, as evidenced by renal impairment or albuminuria.
About two thirds of the individuals with type 2 diabetes mellitus who were diagnosed in this study were anemic. Low hemoglobin levels and tiny red blood cells were the hallmarks of the anemia type that most of these individuals had. Furthermore, In those with type 2 diabetes, we identified a link between the severity of anemia and an increased incidence of albuminuria and chronic renal disease.
REFERENCES
SR Iyer. Type 2 diabetes, ‘express highway’ where is the “U”turn? JAPI. 2003;15:494-500.
Powers AC, Kasper DL, Braunwald E, Fauci A S, Hauser SL, Longo DL, Jamson JL, et al. Harrison’s Principles of Internal Medicine.16th Ed. New York Mc Graw Hill;2005:2152-80.
Zimmet P, Shaw J, Murray S, Sicree R. The diabetes epidemic in full flight: forecasting the future. Diabetes voice. 2003;4:1-16.
Thomas MC, Maclasaac RJ, Tasalamandris C, Molyneaux L, Goubina I, Yue D, et al. Anaemia in patients with type I diabetes. J Clin endocrionl Metab. 2004;89(9):4359-63.
Thomas MC, Maclsaac RJ, Tsalamandris C, Molyneaux L Goubina I, Fulcher G, et al. The burden of anaemia in type 2 diabetes and the role of nephoropathy: a cross sectional audit. Nephrol dial transplant. 2004;19(7):1792-97.
Astor BC, Muntner P, Levin A, Eustace JA, Coresh
J. Association of kidney function with anemia: The Third National Health and Nutrition Examination Survey (1988-1994). Archives internal medicine. 2002;162(12):1401-8.
National anaemia action council. Anaemia: A Hidden Epidemic. Los angles, CA: Health vision communications, Inc. 2002.
Ezenwaka C E, Jones Le Cointe A, Nwagbara E, Seales D, Okali F. Anaemia and Kidney dysfunction
in Caribbean type 2 diabetic patients. Cardiovasc diabetol. 2008;7:25.
Cawood TJ, Buckley U, Murray A Corbett M, Dhillon D, Goodwin B, et al. Prevalence of anaemia in patients with diabetes mellitus. Irish J Med Sci. 2006;175(2):25-7.
Yun Y S, Lee H C, Yoo N C, Song Y D, Lim S K, Kim K R, Hahn J S, et al. Reduced erythropoietin responsiveness to anaemia in diabetic patients before advanced diabetic nephropathy. Diabetic Res Clin Prac. 1999;46:223-9.
Khalil, H.A. Naamat, W.F. (2023) ‘The creation of theoretical frameworks to establish sustainable adoption of e-health in Libya’, Humanitarian and Natural Sciences Journal, 4(7), pp. 207–224. doi:10.53796/hnsj4716.
Djamiatun, K. Naamat, W.F. (2017) ‘Reduce spleen-ifn-γ correlated with CXCL9 levels during cerebral malaria phase in annona muricata-treated swiss mouse study’, Advanced Science Letters, 23(4), pp. 3380–3384. doi:10.1166/asl.2017.9179.
Djamiatun, K., Abdulaziz, Naamat, W.F. (2017) ‘annona muricata associated with increase phytohemaglutinin induced spleen IL-10 production of Swiss mice during cerebral malaria phase’, Advanced Science Letters, 23(4), pp. 3344–3348. doi:10.1166/asl.2017.9161.
Alzrgani, H.A., Naamat, W.F. and Aboughuffah, A.A. (2024) ‘The incidence of calcium deficiency among expectant mothers, study conducted at Zliten Medical Center’, Humanitarian and Natural Sciences Journal, 5(1), pp. 572–589. doi:10.53796/hnsj51/38.