Qaid Hasan Ali Al–Asabe1
PhD Scholar, Faculty of Medicine & Human Sciences, Sana a University-Yemen
Email: qaidm10@gmail.com
HNSJ, 2022, 3(12); https://doi.org/10.53796/hnsj31245
Published at 01/12/2022 Accepted at 20/11/2022
Abstract
Length of stay in hospital is a key performance indicator for hospital management and a key measure of the efficiency, can play a major role in planning for the optimal use of hospital resources. This study aimed to determine the Average Length of Stay (ALOS) and identify factors affecting the patient’s Length of Stay among patients who were discharged from a university of sciences and technology hospital Sana’a, Yemen. We conducted a retrospective cross-sectional study was performed on electronic health records (EHR) of hospitalized patients, including discharged 84,421 patients between April 2014 and September 2019. The data were analysed using Microsoft Excel and IBM SPSS Statistics software version 26.0. Our results showed that the total mean of hospital stay in the USTH was 3.11(days), the associated factors with the LOS were the day of admission (P-value <,000), state of patients at discharge (P-value <,000), No of admission (P-value <,001), department (P-value <,000) and sex of patient (P-value <,000). This data also suggests reducing inappropriate hospital stays, decrease costs and increasing hospital efficiency. Further studies are recommended to identify other clinical, nonclinical, and managerial factors affecting Length of Stay in the same hospital and others.
Key Words: Length of stay; hospital performance; efficiency indicators; discharge patients.
عنوان البحث
مدة بقاء المريض في مستشفى جامعة العلوم والتكنولوجيا, والعوامل المؤثرة,
صنعاء – الجمهورية اليمنية
قائد حسن علي الاصابع1
1 طالب دكتوراه, كلية الطب والعلوم الصحية, جامعة صنعاء, الجمهورية اليمنية
البريد الالكتروني: qaidm10@gmail.com
HNSJ, 2022, 3(12); https://doi.org/10.53796/hnsj31245
تاريخ النشر: 01/12/2022م تاريخ القبول: 20/11/2022م
المستخلص
تعد مدة الإقامة في المستشفى مؤشرًا رئيسيًا للأداء, لإدارة المستشفى ومقياسًا رئيسيًا للكفاءة، ويمكن أن تلعب دورًا رئيسيًا في التخطيط للاستخدام الأمثل لموارد المستشفى. هدفت هذه الدراسة إلى تحديد متوسط مدة الإقامة (ALOS) وتحديد العوامل التي تؤثر على مدة إقامة المريض في المستشفى. أجريت الدراسة في مستشفى جامعة العلوم والتكنولوجيا صنعاء، اليمن. أستخدم البحث المنهج القطعي العرضي وتم استخدام بيانات ثانوية من السجلات الطبية الالكترونية في المستشفى خلال الفترة من عام 2014 حتى 2019. تم تحليل البيانات باستخدام Microsoft Excel وSPSS الإصدار 26.0. أظهرت النتائج أن متوسط فترة الإقامة في المستشفى كان 3.11 (أيام)، وكانت العوامل المرتبطة بـ فترة الإقامة في المستشفى هي: يوم دخول المريض، حالة المريض عند الخروج، رقم الدخول، القسم وجنس المريض, وتوصي الدراسة بتقليل الإقامات غير المناسبة في المستشفى، وخفض التكاليف وزيادة كفاءة المستشفى، ويوصى بإجراء مزيد من الدراسات لتحديد العوامل السريرية وغير السريرية والإدارية الأخرى التي تؤثر على مدة الاقامة في المستشفى وغيرها.
الكلمات المفتاحية: مدة الاقامة؛ أداء المستشفى؛ مؤشرات الكفاءة؛ مرضى الخروج؛
1. Introduction
1-1- background:
Hospital is one of the most important components of a health network. Most of the health care sector’s share from the national GDP is spent in hospitals [1]. Hospital costs have increased. The best way to reduce hospital costs and save expenditures is by improving the efficiency and productivity. The first step in any form of health care system is to improve the performance of hospitals. Thus, we cannot meet that before measuring the current situation of hospital efficiency and productivity. Where productivity is not measured, decision-making becomes exceedingly difficult for policymakers and planners. The majorities of decisions that are made are unscientific and impractical, causing a waste of valuable resources in the health care sector[2].
By reducing Hospital Length of Stay (LOS) we can decrease the cost of hospital and health care services. at the same time LOS is a key performance indicator for hospital management and a key measure of the efficiency[1]. Average LOS refers to the average number of days those patients spend in the hospital to take care, and It is measured by dividing the total of days stayed by all inpatients during a year by the number of admissions or discharges[3]. Moreover LOS continues to remain one of the most popular indices used in assessing hospital performance and efficiency[4]. Therefore, the LOS is an essential indicator to analyse hospital performance[5].
The longer stay in hospital can be indicative to: poor-value care and inefficient hospital processes, also delays in providing treatment; errors and poor-quality care may mean patients need further treatment or recovery time, than the poor care coordination may leave people stuck in the hospital waiting for ongoing care to be arranged(OECD 2021a). The patients’ longer or shorter than the necessary length of stay will influence the cost and quality of provided care firstly. second longer LOS may cause limited resources usages and lower level of service provision to a higher number of people, third; higher pressure for more investment in new treatment centers, another; lower efficiency and higher depreciation of hospital facilities, also more specifically exposure to a hospital infection, complications of re-admission, finally moreover reduction of available resources for patients with critical conditions[7].
Decreased LOS has been associated with decreased risks of opportunistic infections, side effects of medication, with improvements in treatment outcomes and lower mortality rates. Therefore, shorter hospital stays can reduce the burden of medical fees and increase the bed turnover rate, which in turn increases the profit margin of hospitals. In addition , while lowering the overall social costs[8]. The lack of identical guidelines for the optimal length of stay of patients in these wards will lead to longer hospitalization, and thus additional charge on patients as well as hospitals[9].
In 2015, the average length of stay in hospitals for all causes across OECD countries was about eight days, overall. Turkey and Mexico had the shortest stays, with about four days, whereas Japan and Korea had the longest stays, with over 16 days[6]. Some studies in the US found that there were 35.7 million hospital stays in 2016. Overall, the mean LOS was 4.6 days[10]. The average LOS is different from- country to another according to different variables. Several studies and literatures have examined LOS and effective management. They found that multiple variables as related factors affecting patients’ length of stay. Depending on the major goal and studied population, these factors will be different[7].
The most variable have examined as influential factors on the patients’ LOS in the hospitals were age, sex, occupation, and place of residence, also number of previous admissions and cause of referral, another variables the cause of admission, admission on different days of the week and type of insurance, additionally type of admission, type of payment and hospitalization ward, finally moreover the specialty of the physician, and academic degree of the physician[11],[12],[10],[5].
In some studies. The diagnosis was a major factor correlating with the number of days of care, among high frequent diagnoses. which were registered over 250 times. The diagnoses of cerebral infarction, middle cerebral artery with (Mean: 13.42) and infarction of middle cerebral artery territory with (Mean: 13.96) were associated with a higher mean and interquartile range for LOS in hospitals[8]. Other factors affecting patients’ LOS. The most important factors affecting LOS were the number of para-clinical services, specialist consultation count, and clinical ward[13]. Compared with among demographic variables, the only average LOS showed a significant difference between groups of gender, since men had a longer LOS. Mean and median of patients’ LOS in the surgery ward were 3.30±3.71 and 2 days respectively[7].
According to study were done in Victoria, Australia, admissions with prolonged hospitalization included only 9.7% of admissions. but used 44.2% of all hospital bed days. Factors independently associated with prolonged hospitalization included age, female gender, admission from another hospital, admission on the weekend, and the number of admissions in the prior 12 months. They found that patients admitted for surgical reasons were less likely to experience prolonged hospital stay compared to medical admissions[14]. The average LOS in some studies was 13.7 ± 8.9 days. while bivariate analysis showed that a greater proportion of diabetes and hypertension cases had LOS of over 7 days than those who did not have. However, these differences in proportions were not statistically significant[5]. In the middle-income countries. The mean of teaching hospital LOS was 5.45 ± 6.14 days. However age, employment, marital status, history of the previous admission, patient condition at discharge, method of payment, and type of treatment had an impact on LOS[15].
Based on the literature, variables included in different studies,[11], [10], [16], [14],[17]. We determine variables in this study, and commonly are available at the Hospital (Gander, No of admission, department, state of discharge, date of admission and discharge, then LOS as response or dependent variable). We aimed to determine the Average Length of Stay (ALOS), and identify factors affecting the patient’s LOS in a university of sciences and technology hospital Sana a Yemen 2014-2019.
In this study we have two questions, first what is the Average Length of Stay (ALOS) in a university of sciences and technology hospital? second what are the factors affecting the LOS in the university of sciences and technology hospital? And six Hypotheses as following:
- H1: For period of study, LOS differ based on patient’s state of discharge.
- H2: For period of study, LOS differ based on department of patient stayed in.
- H3: For period of study, LOS differ based on NO of admission.
- H4: For period of study, LOS differ based on sex of patients.
- H0: For period of study, there is no difference in LOS based on patient admission day.
- H0: For period of study, there is no difference in LOS based on year of discharge patients.
2. Methods
2.1 Study design, setting, sampling, and data collection
A retrospective cross-sectional study evaluating the hospital (ALOS), and association factors affecting the (LOS) for patients hospitalized in a university of sciences and technology hospital. This hospital is a major private hospital in Sana a, Yemen. The study population was all discharged patients between April 2014 and September 2019, which collected on the defined period were 84,421discharged patient. The data were taken from electronic health records (EHR) of hospitalized patients. The sample included were 69,491 patients. In contrast, we excluded the day case patients that were 14,930.
2.2 Measures
The data collected for the goals of the study were extracted from Hospital EHR using a data report form. The report contained the following data; as the name of the patient, department, and state of patients at discharge, also date of admission, and date of discharge, additionally number of admission and gander added by the researcher. Variables in this study were defined in Table (1) and Table (2(. Hospital bed days were calculated using the dates of admission and discharge, by counting the sum of the number of days spent in the hospital for each inpatient who was discharged during the time of period examined. ALOS measured by dividing the total number of days stayed by all inpatients during a year by the number of admissions or discharges[6].
| Table (1) Distribution of Patients LOS in USTH based on different variables. | |||||||
| No | Variables | n | % | Mean | SD | p-value | |
| Gander | Male | 32190 | 46.3 | 3.3740 | 1.84756 | .000 | |
| Female | 37301 | 53.7 | 2.8932 | 1.72579 | |||
| No of admission | First admission | 51676 | 74.4 | 3.1312 | 1.78413 | .001 | |
| Second admission | 10887 | 15.7 | 3.0644 | 1.79824 | |||
| Third admission or more | 6928 | 10.0 | 3.0831 | 1.90833 | |||
| state of discharge | Improved | 37702 | 54.3 | 2.9642 | 1.73870 | .000 | |
| By doctor order | 22942 | 33.0 | 3.2487 | 1.77954 | |||
| Transfer to other hospital | 78 | .1 | 4.3077 | 2.31487 | |||
| DAMA | 4263 | 6.1 | 3.3045 | 1.92886 | |||
| Death | 2053 | 3.0 | 4.0434 | 2.26176 | |||
| Others | 2453 | 3.5 | 3.0644 | 1.83626 | |||
| Department | Second floor | 5013 | 7.2 | 3.1053 | 1.75769 | .000 | |
| CCU | 3456 | 5.0 | 2.6942 | 1.38440 | |||
| Intermediate care unit | 451 | .6 | 3.6940 | 2.03403 | |||
| ICU | 1462 | 2.1 | 3.9808 | 2.22786 | |||
| VIP Male D | 6717 | 9.7 | 4.0631 | 1.81661 | |||
| VIP Female D | 8646 | 12.4 | 3.6718 | 1.49309 | |||
| General MSMW | 15481 | 22.3 | 3.2148 | 1.79440 | |||
| General MSFW | 16021 | 23.1 | 3.1522 | 1.66549 | |||
| Neuro ICU | 394 | .6 | 4.4898 | 2.35547 | |||
| Neonatal ICU | 3786 | 5.4 | 3.3943 | 1.88523 | |||
| Delivery department | 8064 | 11.6 | 1.2693 | .62315 | |||
| Neonatal ICU | 5013 | 7.2 | 3.1053 | 1.75769 | |||
Source: by researcher
| Table (2) Distribution of Patients LOS in USTH based on different variables. | |||||||
| Variables | N | % | Mean | SD | p-value | ||
| Day of admission | Saturday | 10698 | 15.4 | 3.1698 | 1.78805 | .000 | |
| Sunday | 10800 | 15.5 | 3.0841 | 1.77260 | |||
| Monday | 10731 | 15.4 | 3.0448 | 1.78300 | |||
| Tuesday | 10745 | 15.5 | 3.0781 | 1.80756 | |||
| Wednesday | 10716 | 15.4 | 3.0911 | 1.81679 | |||
| Thursday | 9579 | 13.8 | 3.1025 | 1.80656 | |||
| Friday | 6222 | 9.0 | 3.3300 | 1.81908 | |||
| Year of admission | 2014.00 | 10194 | 14.7 | 3.0901 | 1.87920 | .000 | |
| 2015.00 | 10198 | 14.7 | 3.0040 | 1.81791 | |||
| 2016.00 | 11475 | 16.5 | 3.2001 | 1.80205 | |||
| 2017.00 | 14226 | 20.5 | 3.1532 | 1.77594 | |||
| 2018.00 | 15135 | 21.8 | 3.0880 | 1.76790 | |||
| 2019.00 | 8263 | 11.9 | 3.1560 | 1.75964 | |||
Source: by researcher
Independent Variables: Gander, No of admission, Department, State of discharge, Day of admission, year of admission.
2.3 Inclusion and exclusion criteria
2-3-1-Inclusion criteria:
- All patients admitted to staying in hospital and discharged in the period of study including acute and chronic.
- All medical and surgical discharged patients.
- All delivery discharged patients.
2-3-2-Exclusion criteria
- Day case discharged patients.
- Healthy babies born in a hospital.
2.4 Data analysis
The data were analysed using Microsoft Excel 97-2003 and analytical descriptive IBM SPSS Statistics software version 26.0. Frequency distributions, means, SD, were included in descriptive statistics. Hypotheses were developed appropriately to examine whether independent variables have significant differences in LOS, also ANOVA was used in hypotheses testing.
3. Results
The total of patients was collected 84,421, excluded day-case discharged patients (14,930). The sample was 69,491 patients. This study shows that Female patients were more than half of discharged patients (53.7%), male (46.3%) (Figure 1). The first admission was the most discharged patients 74.4%, compared with the second admission 15.7%, however third admission and more were 10%. The distribution of the state of patients at discharge as a result of this study shows More than half of patients were Improved at discharge 54.3%, while patients discharged by doctor’s order 33%, and DAMA discharge 6.1%, at the same time death patients were 3%, too Transferred patients to another hospital 0.1%, then discharged under the term of others were 3.5%.
Figure (1) Distribution of patients based on gander.
The total mean of hospital stay in the USTH was 3.11(days) for gender in the period of study 2014-2019. The total mean for females was 2.89, compared with the mean of LOS for males was 3.37. In addition, the mean length of stay for discharged patients related to the state of discharge showed that the patients who Transferred to other hospitals were longer LOS of 4.30; the mean LOS of death patients was 4.04; whereas discharged by doctor order was 3.24; DAMA 3.30; others 3.06, and mean LOS for improved patients 2.96. In comparison, the length of stay of discharged patients was carried out by departments and showed that the longest LOS was Neuro ICU by a mean of 4.48, by contrast, 1.26 days for delivery department patients was the shortest LOS department. moreover, details of LOS for discharged patients related to the department are provided in table No (1). Finally, according to the day of admission, results show that the longest LOS was for Friday by a mean of 3.33.
4. discussion
This study aims to identify the (ALOS) and determine factors affecting the patient’s (LOS) between discharged patients. According to the results of this study, the total mean of LOS for discharged patients in USTH -Sana Yemen was 3.11 days, Data cover all inpatient cases (including curative and acute care cases), for the period of study. in comparison with another study[6], the average length of stay in USTH was shorter than the average length of stay in hospitals across OECD countries that which was 7.6 days. furthermore, shorter than the shortest hospital stays in hospitals across OECD countries (Mexico and Turkey about 4 days on average) although the hospitals of OECD countries that were evaluated, curative cases were not included. It can be noticed that male patients who had been discharged from USTH during the period of the study had a longer LOS by a mean of 3.37 (days), compared with female LOS mean of 2.89 (Figure 2). Further, this study showed that the total present of male mortality was 62%. However, female mortality was 38%. Therefore, this distribution for sex mortality may explain the differentiation in LOS between males and females regarding to the state of discharge. The transferred patients to other hospitals have the longer LOS by a mean of 4.30 (days). By contrast, improved patients had the shortest LOS of 2.96 days. While dead patients had a LOS of 4.04 days, patients who were discharged by doctor order LOS were 3.24 days and 3.30 between DAMA discharged patients (Figure 3).
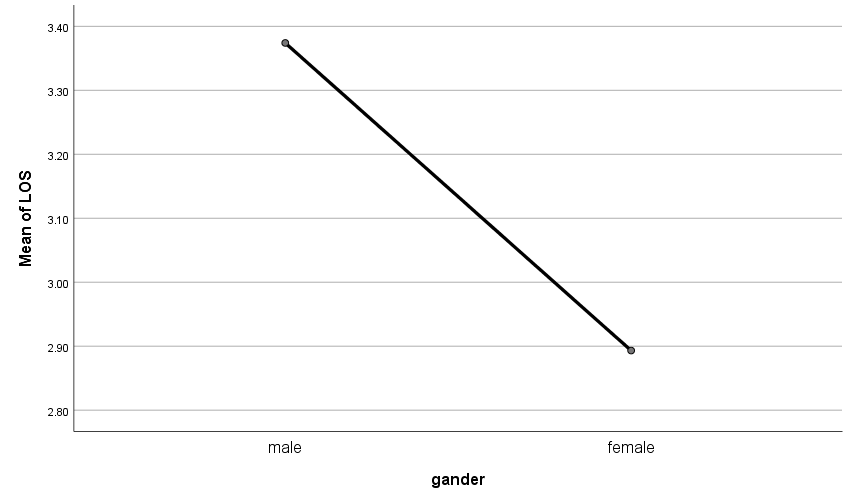
Figure (2) : Length of Stay based on gander of patients
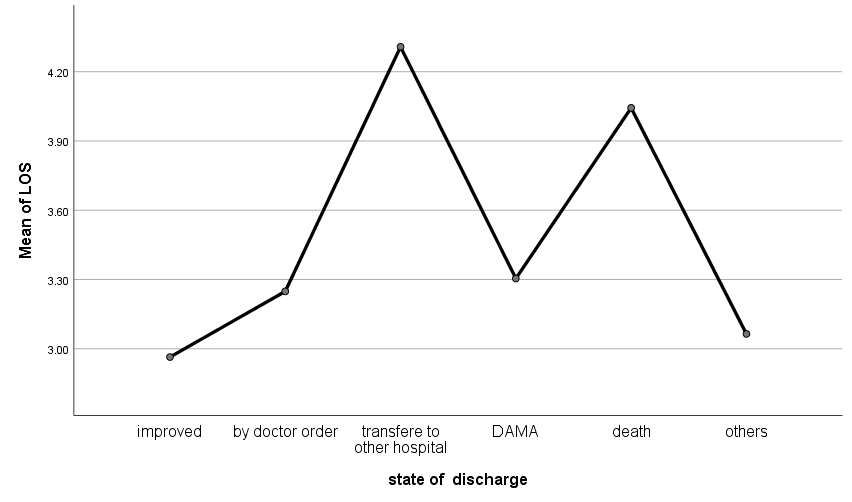
Figure (3) Length of Stay based on state of discharge.
LOS of patients who had the first admission was the longest LOS among all discharged patients related to the No of admission, by contrast, the second admission was the shortest mean of LOS 3.06 (days). while with third admissions or more than 3.08. regarding the department of discharged patients, the neuro ICU had a longer LOS of 4.48 (days) conversely the delivery department had a shorter mean LOS of 1.26 (days) than other departments see (figure 4). In comparison with other Studies, the results of this study showed that there was a significant difference between the sex of patients and their length of stay, and other studies[7],[18]. showed that the sex factor had correlated with LOS. Furthermore, this study found that the factor of the department as (a clinical factor) was correlated with LOS, so the patients who were admitted to Neuro ICU had the longer LOS with a mean of 4.48 days. related to another study[19],[18],[10],[12]. severity of illness and medical complications were the primary issues causing increased LOS in stroke patients, or patients who receiving critical care. likewise, in some studies for stroke patients [20] the mean length of hospital stays showed (28 days). Also, other critical care departments (ICU, NICU) were longer LOS than other departments, it was 3.98(days) in ICU, and 3.69(Days) in the Intermediate Care Unit, finally cardiac care unit patients, were shorter LOS than in VIP Medical-Surgical Departments.
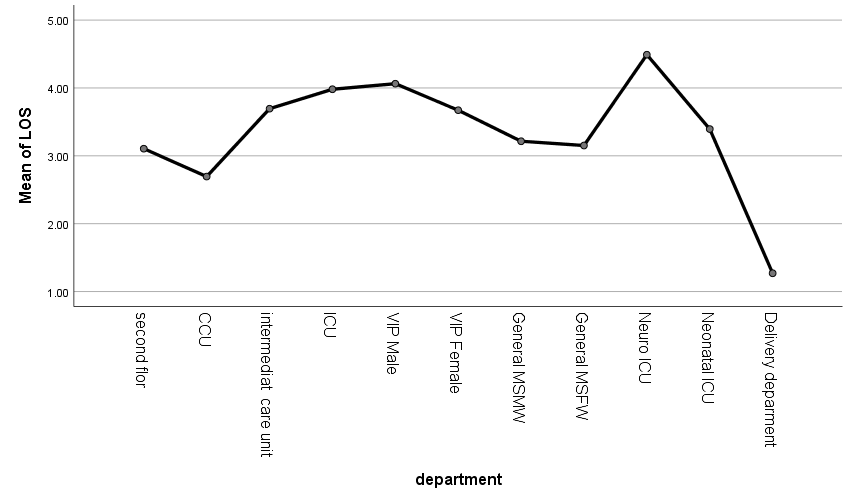
Figure (4) Length of Stay based on department.
The State of discharge in other studies [3], [2], [15], [8], [7], [21], [14] confirmed that the patient condition at discharge effect longer LOS. Likewise, in this study, the result showed that transferred patients to other hospitals have a longer mean LOS of 3.92 days and SD 2.563. USTH as a private hospital the increasing cost and the severity of illness are the main causes for transferring of patients with longer LOS to other hospitals. at the same time, some studies[22] resulted show that patients admitted from other hospitals have a longer length of stay, as a result of complexity of the illness and worsening of these patients, resulting in the inability of the hospital or the primary care center to treat them, because the lack of facilities to provide the patient with the services needed may worsen their condition.
Finally LOS of the patients admitted on Friday were longer LOS than other patients who were admitted on other weekdays, and there is no significant difference between other days because the Friday is (weekend in Yemen) and if the patients need some diagnostic or therapeutic procedures to be done, it will be postponed to another day to be done by specialists staff. similarly In another study [14] LOS of the patients admitted on weekends were longer LOS than other patients. See (figure 5).
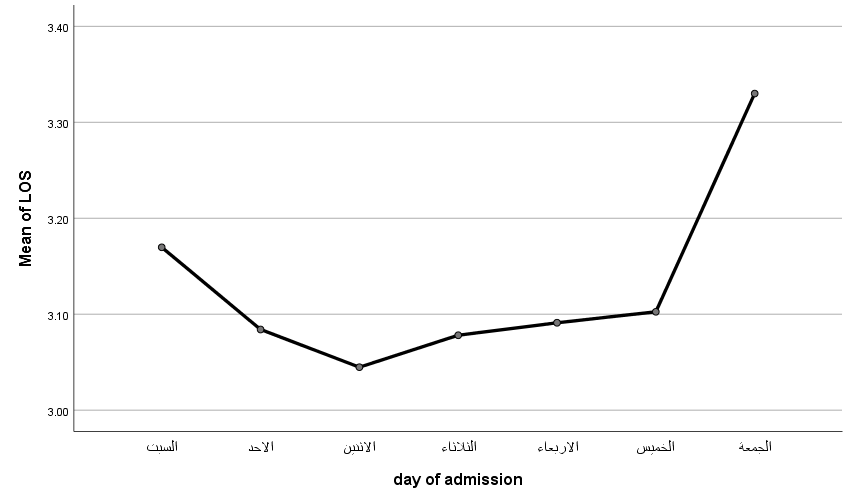
Figure (5) Length of Stay based on day of admission.
Study limitations
This study has several limitations, first according to the unique condition of each hospital. This study has been conducted only in a university of sciences and technology hospital, and other general and private hospital some of them refusing to give data and most of hospitals do not have same data. As a result, the results cannot be generalized to other hospitals. Second the study was conducted using electronic health record database, therefore, the findings are limited to the available variables in the electronic health record of patients. Thus, some influential variables unlisted in record database of discharge patients such as (patients’ diagnosis, age, type of payment, other patients’ demographic data) that might have influenced LOS but not included in our study due to unavailability of data. Thirdly use of coding information for big data.
Conclusion
The results of this study found that the total mean of ALOS in the USTH of Yemen was 3.11(days) shorter than more studies, and many factors significantly associated with longer LOS in hospital, such as sex of patients, Number of admission, state of the patient at discharge, department, and day of admission can be affected on inpatients LOS in USTH of Yemen. Further, studies are recommended to identify other clinical, nonclinical and managerial factors affecting LOS in the same hospital and others (public and private) and providing solutions to reduce inappropriate hospital stay, hospital cost, and increasing efficiency and effectiveness of healthcare services, outcome and to make good decisions for policymakers at the executive level and improve performance of hospitals.
Acknowledgments
This article was a part of a Ph.D. Dissertation supported by Sana a University and university of sciences and technology hospital Sana a Yemen. We should grateful to thank Abdullatif Ghallab for his technical help in analyzing data, language editing assistance. and the hospital’s general manager of USTH Fahmi Al Hakimi for their kind cooperation with the researcher and his agreement to collecting data.
References
[1] E. Kulinskaya, D. Kornbrot, and H. Gao, ‘Length of stay as a performance indicator: robust statistical methodology’, IMA J. Manag. Math., vol. 16, no. 4, pp. 369–381, Oct. 2005, doi: 10.1093/imaman/dpi015.
[2] S. A. Rasool, A. Saboor, and M. Raashid, ‘Measuring Efficiency of Hospitals by DEA: An Empirical Evidence from Pakistan’, International Journal of Public Health Science (IJPHS), vol. 3, no. 2. 2014, doi: 10.11591/ijphs.v3i2.6091.
[3] Organisation for Economic Cooperation and Development (OECD), ‘Health at a Glance 2021’, Nov. 09, 2021. https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2017_health_glance-2017-en.
[4] O. Abdul-Afeez Somotun, K. O. Osungbade, O. O. Akinyemi, T. A. Obembe, and F. I. Adeniji, ‘What factors influence the average length of stay among stroke patients in a Nigerian tertiary hospital?’, Pan African Medical Journal, vol. 26. 2017, doi: 10.11604/pamj.2017.26.228.12249.
[5] S. R. Nietert PJ, Silverstein MD, ‘Hospital Admissions, Length of Stay, Charges’,. 2019, doi: 10.21203/rs.2.14366/v1.
[6] OECD, ‘Hospital discharges and average length of stay | Health at a Glance 2021 : OECD Indicators | OECD iLibrary’, OECD iLibrary. 2021, [Online]. Available: https://www.oecd-ilibrary.org/sites/ae3016b9-en/1/3/5/8/index.html?itemId=/content/publication/ae3016b9-en&_csp_=ca413da5d44587bc56446341952c275e&itemIGO=oecd&itemContentType=book.
[7] T. Baniasadi, M. Ghazisaeedi, M. Hassaniazad, S. Kalhori, and M. Shahi, ‘A Study of Factors Affecting on Patients’ Length of Stay in a Surgical Ward: Toward Optimization by Technology-based Solutions’, 2019, doi: 10.21203/rs.2.14366/v1.
[8] H. Baek, M. Cho, S. Kim, H. Hwang, M. Song, and S. Yoo, ‘Analysis of length of hospital stay using electronic health records: A statistical and data mining approach’, PLoS One, vol. 13, no. 4, Apr. 2018, doi: 10.1371/journal.pone.0195901.
[9] A. Rezaianzadeh, M. Dastoorpoor, M. Sanaei, C. Salehnasab, M. J. Mohammadi, and A. Mousavizadeh, ‘Predictors of length of stay in the coronary care unit in patient with acute coronary syndrome based on data mining methods’, Clinical Epidemiology and Global Health, vol. 8, no. 2. pp. 383–388, 2020, doi: 10.1016/j.cegh.2019.09.007.
[10] W. J. Freeman, A. J. Weiss, and K. C. Heslin, ‘STATISTICAL BRIEF #246 Overview of U.S. Hospital Stays in 2016: Variation by Geographic Region’, 2018. [Online]. Available: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb246-Geographic-Variation-Hospital-Stays.jsp.
[11] T. Baniasadi, K. Kahnouji, N. Davaridolatabadi, and S. Hosseini Teshnizi, ‘Factors affecting length of stay in Children Hospital in Southern Iran’, BMC Health Services Research, vol. 19, no. 1. 2019, doi: 10.1186/s12913-019-4799-1.
[12] Whitney Taiwoa and A. W. and L. Bradleyb, ‘Predicting length of stay in specialist neurological rehabilitation’. 2017, [Online]. Available: https://azure.microsoft.com/en-us/solutions/architecture/predicting-length-of-stay-in-hospitals/.
[13] S. M. Ayyoubzadeh et al., ‘A study of factors related to patients’ length of stay using data mining techniques in a general hospital in southern Iran’, Health Information Science and Systems, vol. 8, no. 1. 2020, doi: 10.1007/s13755-020-0099-8.
[14] R. Ofori-Asenso, D. Liew, J. Mårtensson, and D. Jones, ‘The frequency of, and factors associated with prolonged hospitalization: A multicentre study in Victoria, Australia’, Journal of Clinical Medicine, vol. 9, no. 9. pp. 1–14, 2020, doi: 10.3390/jcm9093055.
[15] O. Khosravizadeh, S. Vatankhah, P. Bastani, R. Kalhor, S. Alirezaei, and F. Doosty, ‘Factors affecting length of stay in teaching hospitals of a middle-income country’, Electronic physician, vol. 8, no. 10. pp. 3042–3047, 2016, doi: 10.19082/3042.
[16] S. M. Ayyoubzadeh et al., ‘A study of factors related to patients’ length of stay using data mining techniques in a general hospital in southern Iran’, Heal. Inf. Sci. Syst., vol. 8, no. 1, Dec. 2020, doi: 10.1007/s13755-020-0099-8.
[17] R. Gardner, G. A. Smith, A.-M. L. Chany, S. A. Fernandez, and L. B. McKenzie, ‘Factors Associated With Hospital Length of Stay and Hospital Charges of Motor Vehicle Crash–Related Hospitalizations Among Children in the United States’, Arch. Pediatr. Adolesc. Med., vol. 161, no. 9, p. 889, Sep. 2007, doi: 10.1001/archpedi.161.9.889.
[18] H. Baek, M. Cho, S. Kim, H. Hwang, M. Song, and S. Yoo, ‘Analysis of length of hospital stay using electronic health records: A statistical and data mining approach’, PLoS ONE, vol. 13, no. 4. 2018, doi: 10.1371/journal.pone.0195901.
[19] J. Sherman, H. David ; Zhu, Service productivity management: Improving service performance using data envelopment analysis (DEA), 2006th edi. New York, NY: Springer, 2006.
[20] A. Van Straten, J. H. P. Van Der Meulen, G. A. M. Van Den Bos, and M. Limburg, ‘Length of hospital stay and discharge delays in stroke patients’, Stroke, vol. 28, no. 1. pp. 137–140, 1997, doi: 10.1161/01.STR.28.1.137.
[21] M. F. Ravangard R, Arab M, Zeraati H, Rashidian A, Akbarisari A, ‘Patients’ Length of Stay in Women Hospital and Its Associated Clinical and Non-Clinical Factors, Tehran, Iran’, Iranian Red Crescent Medical Journal, vol. 13, no. 5. Med. J. Islam. Repub. Iran 30, 36–43 (2016)., 2011.
[22] R. . Nietert, P.J., Silverstein, M.D., & Silver, ‘Hospital Admissions, Length of Stay, Charges, and In-hospital Death Among Patients with Systemic Sclerosis’, J. Rheumatol., vol. 28, no. 9, pp. 2031–2037, 2001.
