Hamza Atia Alzrgani(1), Walid Faraj Naamat(2), Abdullah Ali Aboughuffah(3) Mohmmed Ismail Abosalah(4) (1) Libyan Authority for Scientific Research. Email: Ha.atia@asmarya.edu.ly(2) Department of Medical Laboratory, Faculty of health sciences, Alasmarya Islamic university. Email: w.naamat@asmarya.edu.ly (3) Department of public health, Faculty of health sciences, Alasmarya Islamic university ahmaddd256@asmarya.edu.ly (4) Department of Health Management, Faculty of health sciences, Alasmarya Islamic university Email: m.abosalah@asmarya.edu.ly HNSJ, 2024, 5(1); https://doi.org/10.53796/hnsj51/38 DownloadPublished at 01/01/2024 Accepted at 23/12/2023
Abstract
This paper presents the findings of a study conducted at Zliten Medical Center, investigating the prevalence of calcium deficiency among patients based on age groups, education level and pregnancy times. The study analyzed data from 100 samples and identified key rates and distributions of calcium deficiency within these demographic groups. The results indicated a significant calcium deficiency rate of 57% among patients aged 20 to 30. Furthermore, middle and high school students demonstrated the highest prevalence of calcium deficiency, constituting 46% of the sample. The study also found a substantial 73% higher distribution of women with multiple pregnancies compared to those experiencing their first pregnancy. Within the medical center sample, the third trimester of pregnancy exhibited the highest prevalence of calcium deficiency, reaching 43% based on relative gestational age distribution. Additionally, the analysis revealed a miscarriage rate of 42.25%. These findings highlight the concerning rates of calcium deficiency within specific patient groups and the importance of addressing this issue, particularly among young adults and pregnant women. The study contributes to the understanding of calcium deficiency patterns and emphasizes the need for targeted interventions and preventive measures to mitigate its impact on maternal and fetal health.
Key Words: calcium deficiency, hypocalcemia, pregnant women, miscarriage,
The substrate for bone mineralization is a calcium deficit (Hypocalcemia) a common metabolic disease brought either by calcium loss from circulation or inadequate calcium input into the circulation). If calcium intake is insufficient or calcium losses are high, skeletal mass cannot be developed or preserved. (1)
A calcium shortage serves as the substrate for bone mineralization (hypocalcemia), a common metabolic disease brought on either by calcium loss from circulation or inadequate calcium input into the circulation) (10). Skeletal mass cannot be developed or maintained if calcium intake is inadequate or calcium losses are significant. (2)
Calcium is the primary element of teeth and the skeleton, and calcium is crucial for the activation of muscle-keeping, neurological excitation, and enzymes(7). According to studies, a calcium deficit during pregnancy might worsen postpartum bleeding and result in gestational hypertension(11). When maternal calcium mobilization makes up for the absence of fetal calcium, calcium insufficiency can result in ossification problems and perhaps worsen maternal deficit.(2,27)
According to the World Health Organization (WHO), young individuals should consume 1000 mg of calcium daily, whereas men over 65, postmenopausal women, and children between the ages of 9 and 18 should consume 1300 mg. But not everywhere on the globe does this intake occur(25,26). A significant segment of the population, especially in rural areas of many low-and middle-income nations and territories, does not consume enough calcium in their diets(12,15). The primary dietary sources of calcium are milk, yogurt, and cheese, all of which may be consumed. Kale, broccoli, soft-boned fish like tinned salmon and sardines (17,19)
The risk of developing hypertensive disorders during pregnancy, which is linked to a significant risk of preterm birth and the leading cause of early neonatal and infant mortality, can be reduced by taking calcium supplements during pregnancy(13,21). This is especially true because the fetus’s bone density is affected by calcium levels during pregnancy(8,22). Hyperparathyroidism, which is linked to significant illness for the mother and baby and leads in adverse outcomes such abortion, intrauterine growth retardation, stillbirth, and kidney stones, is the rare cause of high blood calcium levels (hypercalcemia) in pregnant women. (4,22)
Taking calcium supplements while pregnant can lower the chance of developing hypertensive disorders, which are the main cause of early neonatal and infant death and are associated with a considerable risk of preterm delivery(9). This is particularly relevant because calcium levels during pregnancy have an impact on the fetus’s bone density(14,18). The uncommon cause of high blood calcium levels (hypercalcemia) in pregnant women is hyperparathyroidism, which is connected to serious sickness for both the mother and the unborn child and results in undesirable consequences such abortion, intrauterine growth retardation, stillbirth, and kidney stones. (5)
2. PROBLEM OF THE STUDY:
- What is the prevalence of calcium deficiency in pregnant women in Zliten Medical Center?
- How to educate expectant mothers about the value of calcium throughout pregnancy?
3. OBJECTIVES OF THE STUDY:
- Figuring out how common calcium insufficiency is in pregnant women.
- Identifying the groups most at risk for calcium insufficiency in terms of age, education, pregnancy duration, and number of pregnancies.
4. SIGNIFICANCE OF THE STUDY:
It is expected to benefit from this study in:
- Concentrating on the lack of calcium in expectant mothers.
- Health awareness to know the risks of calcium deficiency in pregnant women.
- Health education to identify the importance of nutrition and nutritional supplements for pregnant women and the risks they are exposed to if they are not treated.
5. Paradigm of study:
- Age
- Number of pregnancy
- Months pregnancies
- Qualification
Calcium deficiency rate in pregnant women At Obsterics and gynecology department in Zliten Medical-Center.فics and gynecology department ment
6. Methodology and Procedures
6.1 Research Design:
The design of this study was A cross Sectional study.
6.2 Study Sample:
100 samples were collected for calcium analysis from pregnant women in the obstetrics and gynecology department at Zliten-Medical Center.
6.3 Scope and Limitation of the Study:
This study was limited to the prevalence of calcium deficiency in pregnant women in Zliten Medical Center, this study was conducted in MAY – 2022.
6.4 Procedure:
Procedures: Patients were interviewed at the obstetrics and gynecology department at Zliten Medical Center and some special data were recorded for each case (age, gestational age, number of pregnancies, education). The study sample was a venous blood sample collected in a tube Withe Tube And transfused to the laboratory for analysis by a device ARCHITECT PULS
6.5 Statistical Analysis:
The data used in the study were analyzed was SPSS (statistics package for social sciences) software version 22, To determine the prevalence of calcium deficiency in pregnant women.
6.6 Ethics of Study:
Permission was obtained to conduct the study first and granted by officials at the Zliten Medical Center and the head of the obstetrics and gynecology department in the hospital, obtaining the participant’s consent and giving freedom to withdraw from the research whenever he wants and dealing with information with privacy and confidentiality.
7. Results of Data Analysis.
-
- – Number of Total Respondents for every Category
7.1.1 Age Category
The data gathered from 100 respondents depends on age. The highest percentage rate for the number of respondents in a sample is for the range (20–30) with a 57% percentage. The least percentage rate was for range (Greater Than 40) with 8.0 % percentage that we can see from Table 1.0, Figure 1.0 and Figure 2.0
Table 1.0-Frequencies Table for Age Category
| Age Category | Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|---|
| Less Than 20 | 14 | 14.0 | 14.0 | 14.0 | |
| 20 – 30 | 57 | 57.0 | 57.0 | 71.0 | |
| 31 – 40 | 21 | 21.0 | 21.0 | 92.0 | |
| Greater Than 40 | 8 | 8.0 | 8.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
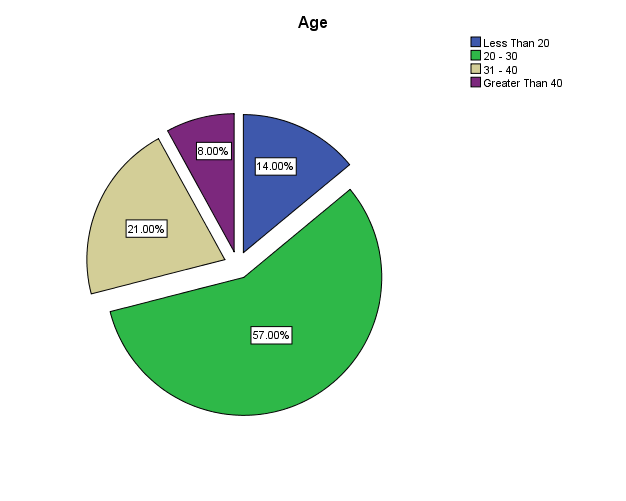
Figure 1.0- Percentage of Respondents for every Age Category
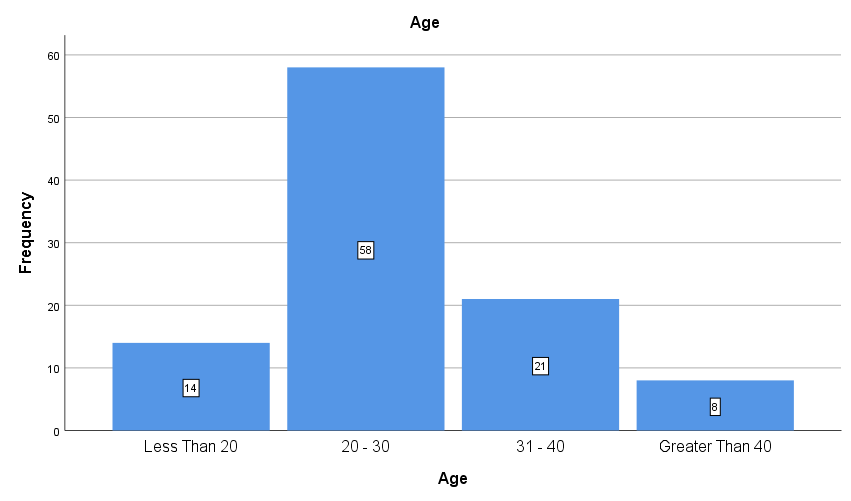
Figure 2.0- Number of Respondents for every Age Category
-
-
- Educational Level
-
From 100 respondents in the sample, depending on educational level, the highest percentage rate for the number of respondents in the sample is for preparatory and secondary levels with 46.0%. The least percentage rate was for uneducated + primary levels, with a 16.0% percentage, as we can see from Table 2.0, Figure 3.0, and Figure 4.0.
Table 2.0-Frequencies Table for Educational Level Category
| Educational Level | Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|---|
| Uneducated + primary | 16 | 16.0 | 16.0 | 16.0 | |
| Preparatory + Secondary | 46 | 46.0 | 46.0 | 62.0 | |
| University | 38 | 38.0 | 38.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
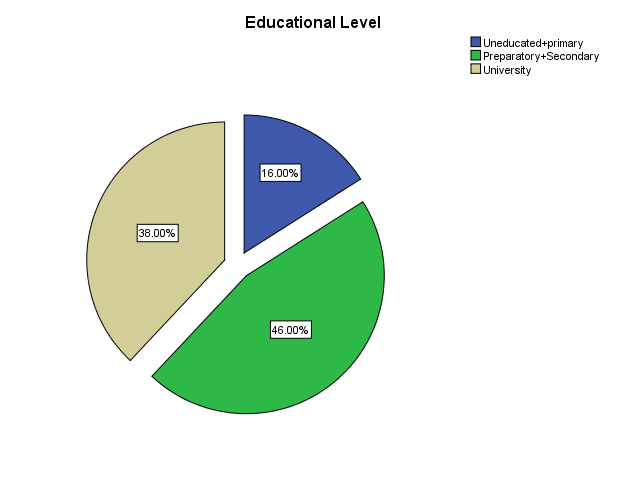
Figure 3.0- Percentage of Respondents for every Educational Level Category
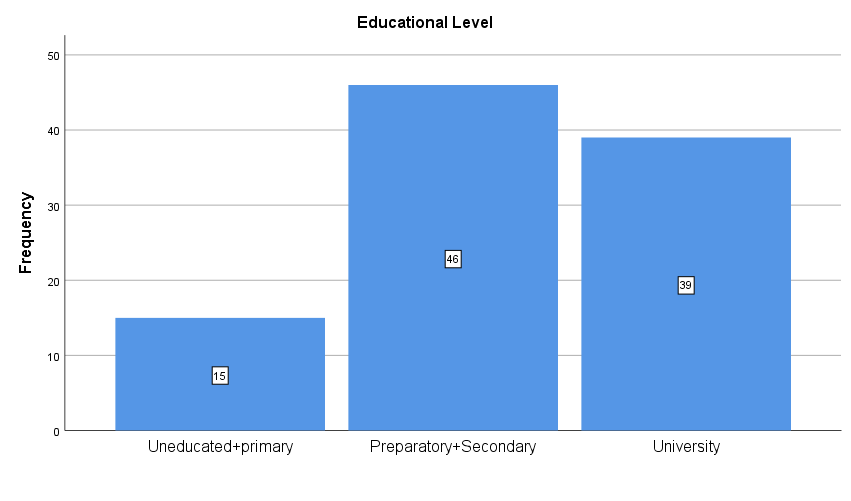
Figure 4.0- Number of Respondents for every Educational Level Category
-
-
- Pregnancy Times
-
From 100 respondents in the sample, depending on pregnancy times, the highest percentage rate for the number of respondents in the sample is for Multi Gravida with 73.0 percent. Table 3.0, Figure 5.0, and Figure 6.0 show that the percentage of Primary Gravida was 27.0%.
Table 3.0-Frequencies Table for Pregnancy Times Category
| Pregnancy Times | Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|---|
| Primary Gravida | 27 | 27.0 | 27.0 | 27.0 | |
| Multi Gravida | 73 | 73.0 | 73.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
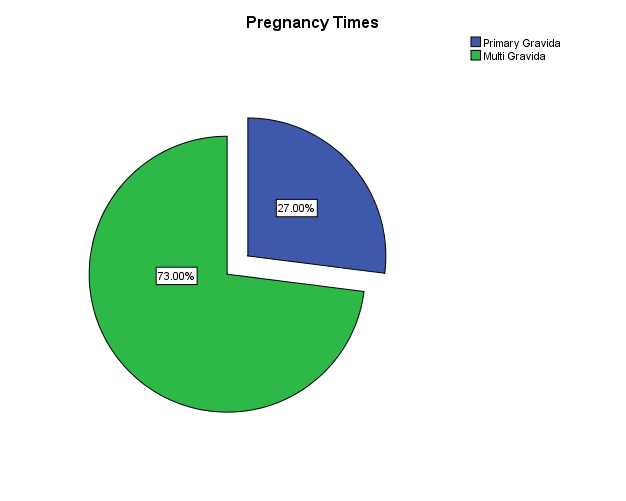
Figure 5.0- Percentage of Respondents for Pregnancy Times Category
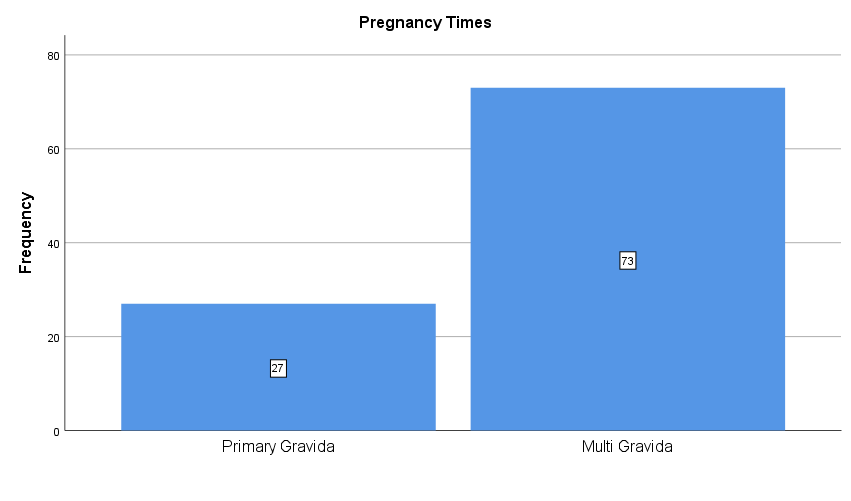
Figure 6.0- Number of Respondents for Pregnancy Times Category
-
-
- Miscarriage
-
From 100 respondents in the sample, depending on miscarriage, the highest percentage rate for the number of respondents in the sample is for (No Miscarriage) with 57.75 %. Table 4.0, Figure 7.0, and Figure 8.0 show that the miscarriage rate was 42.25 percent.
Table 4.0-Frequencies Table for Miscarriage Category
| Miscarriage Category | Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|---|
| No Miscarriage | 73 | 73.0 | 73.0 | 73.0 | |
| Miscarriage | 27 | 27.0 | 27.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
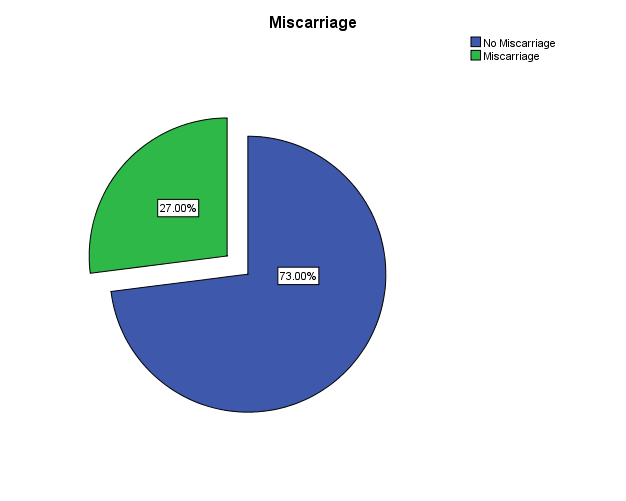
Figure 7.0- Percentage of Respondents for Miscarriage Category
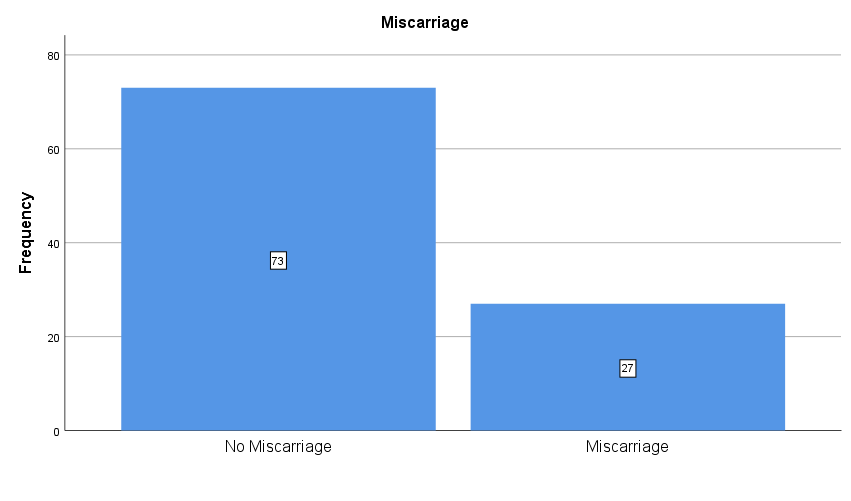
Figure 8.0- Number of Respondents for Miscarriage Category
-
-
- Pregnancy Stages
-
From 100 respondents in the sample, depending on pregnancy stages, the highest percentage rate for the number of respondents in the sample is for (6–9 Months) with a 43.0 percentage. The least one was 1-3 months, with a 21.0 % percentage that we can see from Table 5.0, Figure 9.0, and Figure 10.0.
Table 5.0-Frequencies Table for Pregnancy Stages Category
| Stages Category | Frequency | Percent | Valid Percent | Cumulative Percent | |
| 1-3 Months | 21 | 21.0 | 21.0 | 21.0 | |
| 3-6 Months | 36 | 36.0 | 36.0 | 57.0 | |
| 6-9 Months | 43 | 43.0 | 43.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
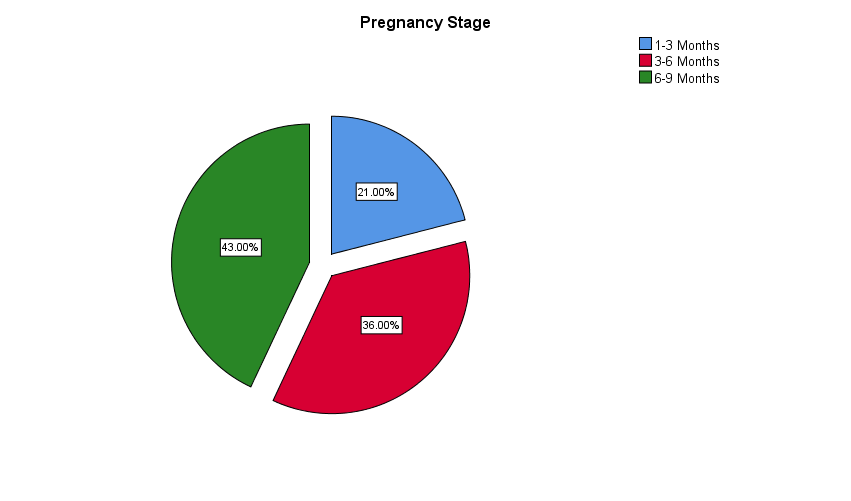
Figure 9.0- Percentage of Respondents for Pregnancy Stages Category
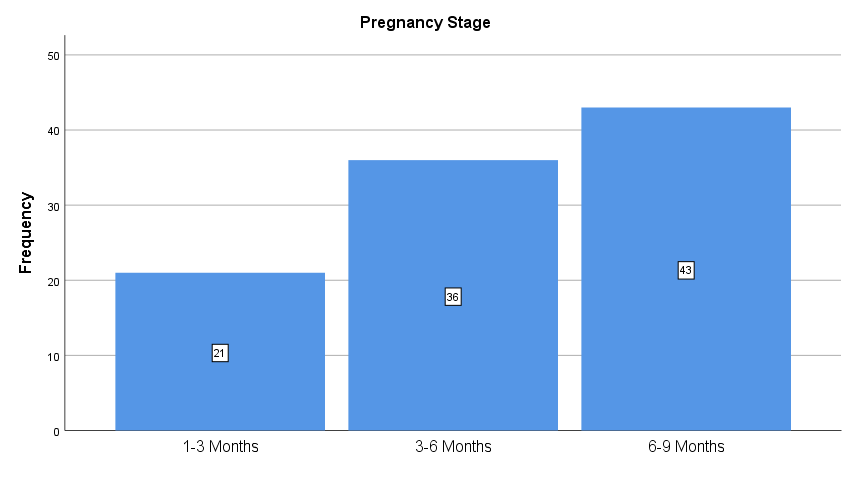
Figure 10.0- Number of Respondents for Pregnancy Stages Category
-
-
- Calcium Range (Hypocalcemia)
-
From 100 respondents in the sample, depending on Calcium Range, the highest percentage rate for data of respondents in the sample is for (Normal (>=8.5)) with 53.0 % percentage. The least one was Less than 8.5 (Hypocalcemia) was at a 47.0 % percentage as we can see from Table 5.0, Figure 9.0 and Figure 10.0.
Table 6.0-Frequencies Table for Calcium Range Category
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
| Less than 8.5 (Hypocalcemia) | 47 | 47.0 | 47.0 | 47.0 | |
| Normal (>=8.5) | 53 | 53.0 | 53.0 | 100.0 | |
| Total | 100 | 100.0 | 100.0 | ||
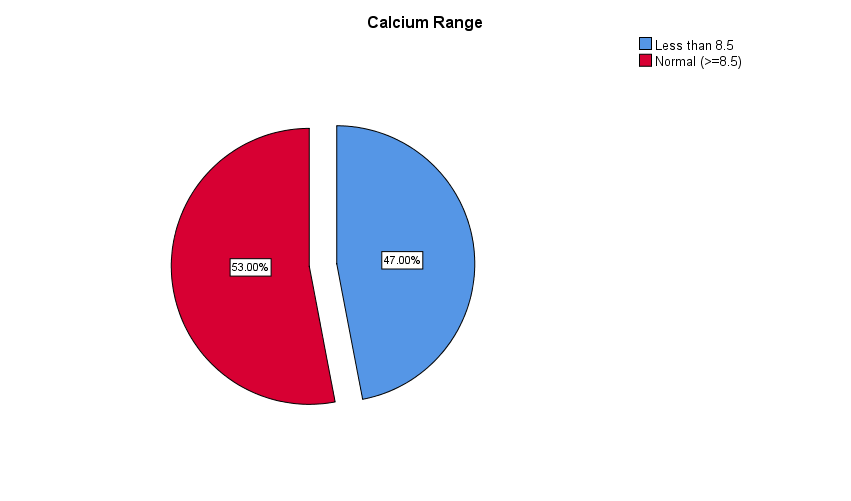
Figure 11.0- Percentage of Respondents for Calcium Range Category
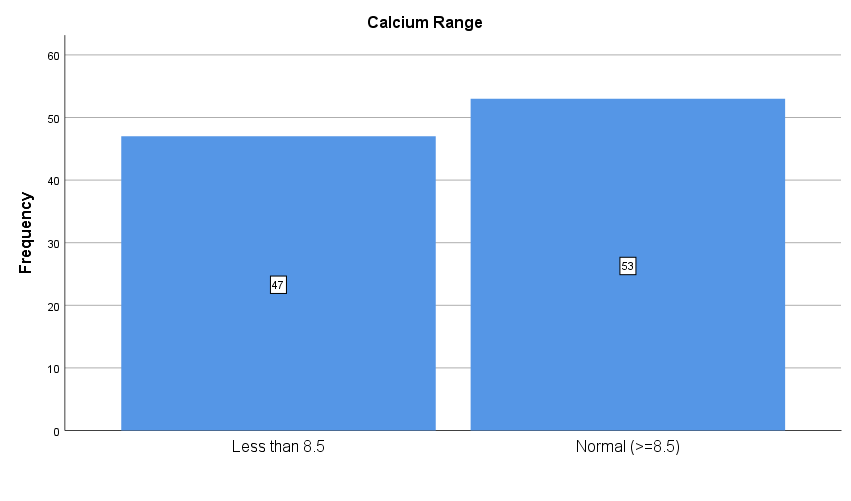
Figure 12.0- Number of Respondents for Calcium Range Category
7.2 – Distribution of Hypocalcemia on Respondents for every Category
As shown from Table 6.0 and Figure 12.0, we can see the number of Respondents who have a Hypocalcemia was 47 Respondents, The Distribution of these respondents on various Categories are as flows:
7.2.1- Distribution of Hypocalcemia on Age Category
The highest percentage rate of hypocalcemia was in the range (20–30) with 57%, and the least percentage rate was for the range (greater than 40) with 11%, as we can see from Table 7.0 and Figure 13.0.
| Age | Less Than 20 | 20 – 30 | 31 – 40 | Greater Than 40 |
| Hypocalcemia (%) | 15 % | 57 % | 17 % | 11 % |
Table 7.0- Percentage of Hypocalcemia depends on Age Category
Figure 13.0- Percentage of Hypocalcemia depends on Age Category
7.2.2- Distribution of Hypocalcemia on Educational Levels Category
The highest percentage rate of hypocalcemia was at level (Preparatory + Secondary) with 49%, and the least percentage rate was at level (Uneducated + Primary) with 17%, as we can see from Table 8.0 and Figure 14.0.
| Educational Levels | Uneducated + primary | Preparatory + Secondary | University |
| Hypocalcemia (%) | 17% | 49% | 34% |
Table 8.0- Percentage of Hypocalcemia depends on Educational Levels Category
Figure 14.0- Percentage of Hypocalcemia depends on Educational Levels Category
7.2.3- Distribution of Hypocalcemia on Pregnancy Stages Category
The highest percentage rate of hypocalcemia was on stage (6–9 months) with 45%. The least percentage rate was for stage (1-3 months) with 15%, as we can see from Table 8.0 and Figure 14.
Table 9.0- Percentage of Hypocalcemia depends on Pregnancy Stages Category
| Pregnancy Stages | 1-3 Months | 3-6 Months | 6-9 Months |
| Hypocalcemia (%) | 15% | 40% | 45% |
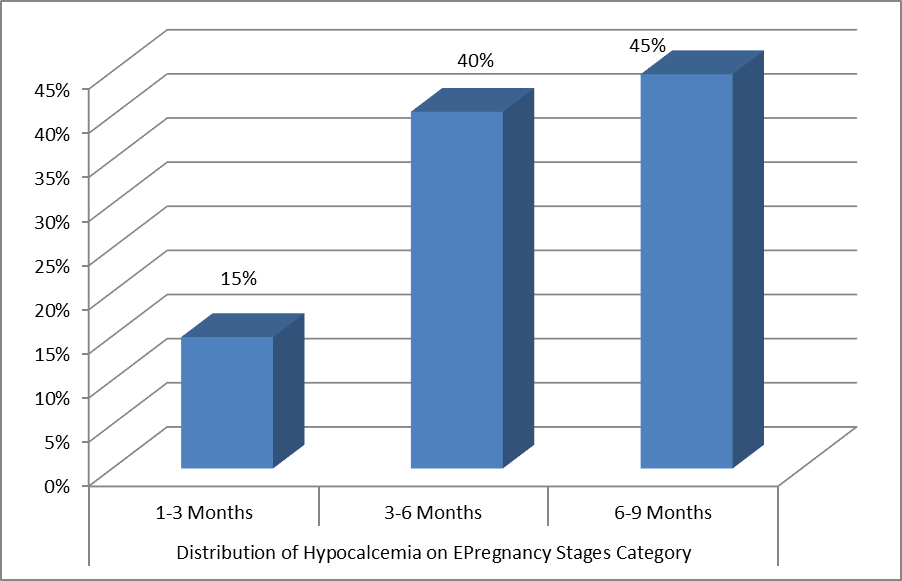
Figure 15.0- Percentage of Hypocalcemia depends on Pregnancy Stages Category
7.2.4- Distribution of Hypocalcemia on Pregnancy times Category
The highest percentage rate of hypocalcemia was in (Multi Gravida) with 77%, and the least percentage rate was for (Primary Gravida) with 23%, as we can see from Table 10.0 and Figure 15.0
Table 10.0- Percentage of Hypocalcemia depends on Pregnancy times Category
| Pregnancy Times | Primary Gravida | Multi Gravida |
| Hypocalcemia (%) | 23% | 77% |
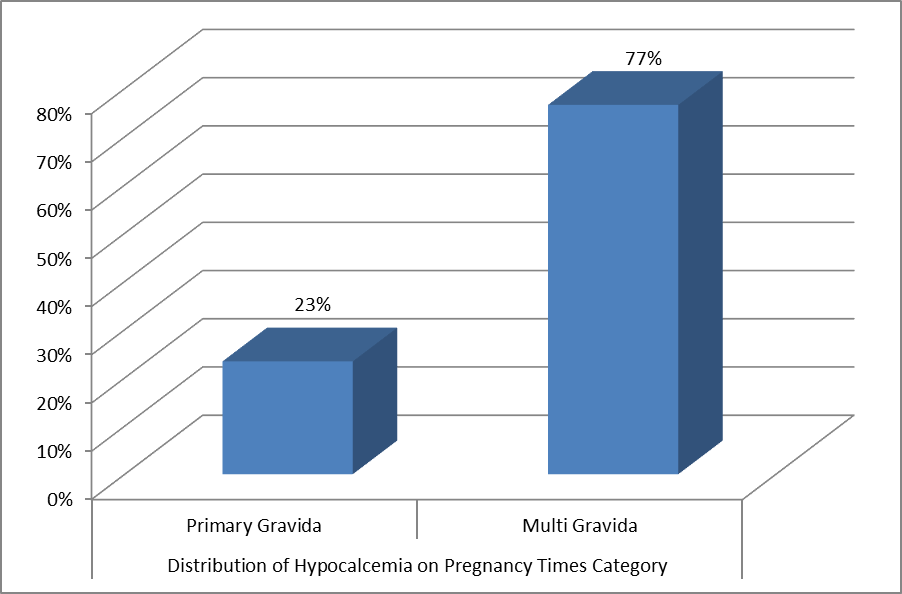
Figure 16.0- Percentage of Hypocalcemia depends on Pregnancy Times Category
7.2.5- Distribution of Hypocalcemia on Miscarriage Category
The highest percentage rate of hypocalcemia was in (No Miscarriage) with 77%, and the least percentage rate was for (Miscarriage) with 23%, as we can see from Table 11.0 and Figure 16.0
Table 11.0- Percentage of Hypocalcemia depends on Miscarriage Category
| Miscarriage | No Miscarriage | Miscarriage |
| Hypocalcemia (%) | 77% | 23% |
Figure 17.0- Percentage of Hypocalcemia depends on Miscarriage Category
8. Conclusion
The results of the study can be summarized as follows: First, after analyzing the data of 100 samples collected from Zliten Medical Center, it was concluded that there was a 57% rate of calcium deficiency among patients aged 20 to 30 years. Secondly, the highest percentage of calcium deficiency patients in the sample was middle and high school students, at 46%. Third, the percentage distribution of women with multiple pregnancies was 73% higher than that of women waiting for the first time in the medical center sample. Fourth, the third trimester of pregnancy witnessed the highest prevalence of calcium deficiency at 43%, based on the relative distribution of the gestational age group at the medical center. Finally, the distribution revealed a miscarriage rate of 42.25%.
- References
- Akhtar, S., Begum, S., & Ferdousi, S. (2011). Calcium And Zinc Deficiency In Preeclamptic Women. J Bangladesh Soc Physiol, 6(2), 94-99.
- Aboughuffah, A. A., Algeesh, S. S., Abosalah, M. I., Alzrgani, H. A., & Naamat, W. F. (2022). Evaluation of level awareness of pregnant women on anemia during pregnancy in “zliten medical center.” Humanitarian and Natural Sciences Journal, 3(11). doi:10.53796/hnsj31136
- Ajong, A. B., Kenfack, B., Mbulli Ali, I., Yakum, M. N., Aljerf, L., & Telefo, P. B. (2020). Hypocalcaemia and calcium intake in Pregnancy: A research protocol for critical Analysis of risk factors, maternofoetal Outcomes and evaluation of diagnostic Methods in a third-category health facility, Cameroon. Published: November 5, 2020.
- Almaghamsi, A., Almalki, M. H., & Buhary, B. M. (2018). Hypocalcemia in Pregnancy. Oman Medical Journal, 33(3), 238–246.
- Bahrami, A., Bahrami-Taghanaki, H., Afkhamizadeh, M., Avan, A., Khorasani, Z. M., Esmaili, H., Amin, B., Jazebi, S., Kamali, D., Ferns, G. A., Sadeghi, H. R., & Ghayour-Mobarhan, M. (2018). Menstrual disorders and premenstrual symptoms in adolescents: prevalence and relationship to serum calcium and vitamin D concentrations. Journal of Obstetrics and Gynaecology, 38(7), 985-990.
- Djamiatun, K., Abdulaziz, K. M. A., Naamat, W. F. A., Kristina, T. N., & Nugroho, D. (2017). Annona muricata Associated with Increase Phytohemaglutinin Induced Spleen IL-10 Production of Swiss Mice During Cerebral Malaria Phase. Advanced Science Letters, 23(4), 3344-3348. https://doi.org/10.1166/asl.2017.9161
- Djamiatun, K., Naamat, W. F. A., Dharmana, E., Wijayahadi, N., & Nugroho, D. (2017). Reduce Spleen-IFN-γ Correlated with CXCL9 Levels During Cerebral Malaria Phase in Annona muricata-Treated Swiss Mouse Study. Advanced Science Letters, 23(4), 3380-3384. https://doi.org/10.1166/asl.2017.9179
- Farveen, W., Abosalah, M. I., Naamat, W. F., Elgenaidi, A. R., & Mustafa, A. B. (2022). Knowledge about the Dietary and Drugs Used in Coronary Heart Disease and Its Assessment in Misrata Hospital. Journal of Drug and Alcohol Research.
- Jouanne, M., Oddoux, S., Noël, A., & Voisin-Chiret, A. S. (2021). Nutrient Requirements during Pregnancy and Lactation. Nutrients, 13(2), 692. https://doi.org/10.3390/nu13020692.
- Shen, P.-J., Gong, B., Xu, F.-Y., & Luo, Y. (2015). Four trace elements in pregnant women and their relationships with adverse pregnancy outcomes. European Review for Medical and Pharmacological Sciences, 19, 4690-4697.
- Shkembi, B., & Huppertz, T. (2022). Calcium Absorption from Food Products: Food Matrix Effects. Nutrients, 14(1), 180. https://doi.org/10.3390/nu14010180
- Kumar, A., & Kaur, S. (2017). Calcium: A Nutrient in Pregnancy. The Journal of Obstetrics and Gynecology of India, 67(5), 319-322.
- Shlisky, J., Mandlik, R., Askari, S., & others. (2022). Calcium deficiency worldwide: prevalence of inadequate intakes and associated health outcomes. Annals of the New York Academy of Sciences, 1505(1), 1-21.
- Pu, F., Chen, N., & Xue, S. (2016). Calcium intake, calcium homeostasis and health. Food Science and Human Wellness, 5, 8-16.
- Calcium homeostasisSouthern South African Journal of Anaesthesia and Analgesia. 2020
- Hypocalcemia Goyal A, Anastasopoulou C, NGU M, et al. Last Update: August 8, 2021.
- Calcium Intake and Health Gabriela Cormick 1,2,3,* and Jose M Belizán 1 Published: 15 July 2019.
- Pepe, J., Colangelo, L., Biamonte, F., Sonato, C., Danese, V. C., Cecchetti, V., Occhiuto, M., Piazzolla, V., De Martino, V., Ferrone, F., Minisola, S., & Cipriani, C. (2020). Diagnosis and management of hypocalcemia. Received: 15 February 2020 / Accepted: 18 April 2020.
- Krueger, D., & Tasota, F. J. (2003). Keeping an eye on calcium levels. Nursing, 33(6), 68-70. (Updated June 1, 2020).
- Naamat, W. F. A., Kisdjamiatun, K., & Kristina, T. N. (2015). The Effectivity of Annona muricata to Reduce IL-12 Level and Number of Leukocyte and Improve Monocyte Percentage (Study in Cerebral Malaria of Swiss Albino Mice) [Master’s thesis, Universitas Diponegoro].
- Njau, M., Mujuni, F., Chibwe, E., Kiritta, R., & Matovelo, D. (2022). Hypocalcaemia in Pregnancy: Diagnosis Challenges in Low Resource Settings. Department of Obstetrics and Gynecology, Bugando Medical Centre, Catholic University of Health and Allied Sciences, Mwanza, Tanzania. Published date: 20 April 2022.
- World Health Organization. (2018). Recommendation: Calcium supplementation during pregnancy for the prevention of pre-eclampsia and its complications. Geneva.
- Khadilkar, A., Khadilkar, V., Chinnappa, J., Rathi, N., Khadgawat, R., Balasubramanian, S., Parekh, B., & Jog, P. (2017, May 20). Prevention and Treatment of Vitamin D and Calcium Deficiency in Children and Adolescents: Indian Academy of Pediatrics (IAP) Guidelines.
- Oudah, N. N., Abdulbari, A. S., & Hameed, N. J. (2022). Serum Electrolytes Levels in Third Trimester Pregnant Women: A Case-Control Study in Diyala Province in Iraq. Egyptian Journal of Chemistry, 65(8), 31-34.
- Hofmeyr, G.J., Manyame, S., Medley, N., & Williams, M.J. (2019). Calcium supplementation commencing before or early in pregnancy, for preventing hypertensive disorders of pregnancy. Cochrane Database of Systematic Reviews.
- World Health Organization. (2019). Nutritional rickets: A review of disease burden, causes, diagnosis, prevention and treatment.
- World Health Organization. (2013). Guideline: Calcium supplementation in pregnant women.
